PREGNANCY:
Most of the time, you won't know the exact day you got pregnant. Your doctor will count the start of your pregnancy from the first day of your last menstrual period. That's about 2 weeks ahead of when conception happens.
Here's a primer on conception:
Each
month inside your ovaries, a group of eggs starts to grow in small,
fluid-filled sacs called follicles. Eventually, one of the eggs erupts
from the follicle (ovulation). It usually happens about 2 weeks before your next period.
Hormones Rise
After
the egg leaves the follicle, the follicle develops into something
called the corpus luteum. The corpus luteum releases a hormone that
helps thicken the lining of your uterus, getting it ready for the egg.
The Egg Travels to the Fallopian Tube
After the egg is released, it moves into the fallopian tube. It stays there for about 24 hours, waiting for a single sperm to fertilize it. All this happens, on average, about 2 weeks after your last period.
If the Egg Isn't Fertilized
If
no sperm is around to fertilize the egg, it moves through the uterus
and disintegrates. Your hormone levels go back to normal. Your body
sheds the thick lining of the uterus, and your period starts.
Fertilization
If
one sperm does make its way into the fallopian tube and burrows into
the egg, it fertilizes the egg. The egg changes so that no other sperm
can get in.
At the instant of fertilization, your baby's genes and sex are set. If the sperm has a Y chromosome, your baby will be a boy. If it has an X chromosome, the baby will be a girl.
The
egg stays in the fallopian tube for about 3 to 4 days. But within 24
hours of being fertilized, it starts dividing fast into many cells. It
keeps dividing as it moves slowly through the fallopian tube to the
uterus. Its next job is to attach to the lining of uterus. This is
called implantation.
Some women notice spotting (or
slight bleeding) for 1 or 2 days around the time of implantation. The
lining of the uterus gets thicker and the cervix is sealed by a plug of mucus. It will stay in place until the baby is ready to be born.
Within 3 weeks, the cells begin to grow as clumps, and the baby's first nerve cells have already formed.
Pregnancy Hormones
A pregnancy hormone known as hCG is in your blood from the time of conception. This is the hormone detected in a pregnancy test.
Usually it takes 3 to 4 weeks from the first day of your last period
for the levels of hCG to be high enough to be found by the tests.
Pregnancy Symptoms
Are you wondering if you might be pregnant? The only way to know for sure is by taking a pregnancy test.
But there are early symptoms of pregnancy that may point to the possibility. Here's what to look for.
Do All Women Get Early Symptoms of Pregnancy?
Every woman is different. So are her experiences of pregnancy. Not every woman has the same symptoms or even the same symptoms from one pregnancy to the next.
Also, because the early symptoms of pregnancy are often like what happens right before and during menstruation, those symptoms aren't always recognized.
What
follows is a description of some of the most common early symptoms of
pregnancy. You should know that these symptoms may be caused by other
things besides being pregnant. So the fact that you notice some of these
symptoms does not necessarily mean you are pregnant. The only way to
tell for sure is with a pregnancy test.
Spotting and Cramping
A few days after conception, the fertilized egg attaches itself to wall of the uterus. This can cause one of the earliest signs of pregnancy -- spotting and, sometimes, cramping.
That's called implantation bleeding. It occurs anywhere from six to 12 days after the egg is fertilized.
The cramps
resemble menstrual cramps, so some women mistake them and the bleeding
for the start of their period. The bleeding and cramps, however, are
slight.
Besides bleeding, a woman may notice a white, milky discharge from her vagina. That's related to the thickening of the vagina's walls, which starts almost immediately after conception. The increased growth of cells lining the vagina causes the discharge.
This
discharge, which can continue throughout pregnancy, is typically
harmless and doesn't require treatment. But if there is a bad smell
related to the discharge or a burning and itching sensation, tell your doctor so they can check on whether you have a yeast or bacterial infection.
Breast Changes
Breast changes are another very early sign of pregnancy. A woman's hormone levels rapidly change after conception. Because of the changes, her breasts
may become swollen, sore, or tingly a week or two later. Or they may
feel heavier or fuller or feel tender to the touch. The area around the
nipples, called the areola, may also darken.
Other things could cause breast changes. But if the
changes are an early symptom of pregnancy, keep in mind that it is going
to take several weeks to get used to the new levels of hormones. But
when it does, breast pain should ease up.
Feeling very tired is normal in pregnancy, starting early on.
A woman can start feeling unusually fatigued as soon as one week after conceiving.
Why? It's often related to a high level of a hormone called progesterone, although other things -- such as lower levels of blood sugar, lower blood pressure, and a boost in blood production -- can all contribute.
If fatigue is related to pregnancy, it's important to get plenty of rest. Eating foods that are rich in protein and iron can help offset it.
Morning sickness is a famous symptom of pregnancy. But not every pregnant woman gets it.
The exact cause of morning sickness is not known but pregnancy hormones likely contribute to this symptom. Nausea during pregnancy may occur at any time of the day but most commonly in the morning.
Also,
some women crave, or can't stand, certain foods when they become
pregnant. That's also related to hormonal changes. The effect can be so
strong that even the thought of what used to be a favorite food can turn
a pregnant woman's stomach.
It's possible that the nausea,
cravings, and food aversions can last for the entire pregnancy.
Fortunately, the symptoms lessen for many women at about the 13th or
14th week of their pregnancy.
In the meantime, be sure to eat a healthy diet so that you and your developing baby get essential nutrients. You can talk to your doctor for advice on that.
The most obvious early symptom of pregnancy -- and the one that prompts most women to get a pregnancy test -- is a missed period. But not all missed or delayed periods are caused by pregnancy.
Also, women can experience some bleeding during pregnancy.
If you are pregnant, ask your doctor what you should be aware of with
bleeding. For example, when is bleeding normal and when is it a sign of
an emergency?
There are reasons, besides pregnancy, for missing a period. it might be that you gained or lost too much weight. Hormonal problems, fatigue, or stress are other possibilities. Some women miss their period when they stop taking birth control pills. But if a period is late and pregnancy is a possibility, you may want to get a pregnancy test.
Other Early Symptoms of Pregnancy
Pregnancy brings changes in your hormonal balance. And that can cause other symptoms..
- Frequent urination. For many women, this starts around the sixth or eighth week after conception. Although this could be caused by a urinary tract infection, diabetes, or overusing diuretics, if you're pregnant, it's most likely due to hormonal levels.
- Constipation. During pregnancy, higher levels of the hormone progesterone can make you constipated. Progesterone causes food to pass more slowly through your intestines. To ease the problem, drink plenty of water, exercise, and eat plenty of high-fiber foods.
- Mood swings. These are common, especially during the first trimester. These are also related to changes in hormones.
- Headaches and back pain. Many pregnant women report frequent mild headaches, and others experience chronic back pain.
- Dizziness and fainting. These may be related to dilating blood vessels, lower blood pressure, and lower blood sugar.
A
pregnant woman could have all of these symptoms, or maybe have only one
or two. If any of these symptoms become bothersome, talk with your
doctor about them so you can make a plan to offset them.
Pregnancy Tests
A pregnancy test may let you know, one way or the other, if you are pregnant.
Here are answers to some of the most common questions about pregnancy tests.
What is a pregnancy test and how does it work?
Pregnancy tests are designed to tell if your urine or blood contains a hormone called human chorionic gonadotropin (hCG). This hormone is produced right after a fertilized egg attaches to the wall of a woman's uterus.
This
usually happens -- but not always -- about six days after
fertilization. If you're pregnant, levels of hCG continue to rise
rapidly, doubling every two to three days.
What types of pregnancy tests are available?
Two main types of pregnancy tests can let you know if you're pregnant: urine tests and blood tests.
Urine tests can be done at home or in a doctor's office. Many women first choose a home pregnancy test to take about a week after a missed period. Home pregnancy tests are private and convenient.
These
products come with instructions. Follow them closely for the most
accurate results. After testing, you can confirm results by seeing your
doctor, who can perform even more sensitive pregnancy tests.
Blood tests
are done at your doctor's office, but are used less often than urine
tests. These tests can detect pregnancy earlier than a home pregnancy
test, or about six to eight days after ovulation. But with these tests, it takes longer to get the results than with a home pregnancy test.
Two types of blood pregnancy tests are available:
A qualitative hCG test
simply checks to see if hCG is present. It gives a "yes" or "no" answer
to the question, "Are you pregnant?" Doctors often order these tests to
confirm pregnancy as early as 10 days after a missed period. However, some of these tests can detect hCG much earlier.
A quantitative hCG test
(beta hCG) measures the exact amount of hCG in your blood. It can find
even very low levels of hCG. Because these pregnancy tests can measure
the concentration of hCG, they may be helpful in tracking any problems
during pregnancy. They may also (in combination with other tests) be
used to rule out a tubal (ectopic) pregnancy or to monitor a woman after
a miscarriage when hCG levels fall rapidly.
How accurate are pregnancy tests?
You
should know that waiting at least a week after a missed period may give
you the most accurate result. Results may also be more accurate if you
do the test first thing in the morning, when your urine is more
concentrated.
Urine home pregnancy tests are about 97% accurate. Blood tests are even more accurate than this.
How accurate a home pregnancy test is depends upon:
- How closely you follow instructions.
- When you ovulate in your cycle and how soon implantation occurs.
- How soon after pregnancy you take the test.
- The sensitivity of the pregnancy test.
Is it expensive or hard to do a home pregnancy test (HPT)?
You
can buy a home pregnancy test in a drugstore without a prescription.
The cost depends on the brand. But most tests are relatively inexpensive
--
Home pregnancy tests are quick
and easy to use. They are also very accurate if you carefully follow
directions. These pregnancy tests all work in a similar way. You test
the urine in one of these ways:
- Hold the test's stick in your urine stream.
- Collect urine in a cup and then dip the test's stick into it.
- Collect urine in a cup and use a dropper to put urine into another container.
With
all of these techniques, you need to wait a few minutes before seeing
the results. Results may show up as a line, a color, or a symbol such as
a "+" or "-" sign. Digital tests produce the words "pregnant" or "not
pregnant."
If you have any questions about the
pregnancy test or the results, call your doctor or the telephone number
listed with the home pregnancy test.
What do the pregnancy test results mean?
It's important to know what a positive or negative result means.
If you get a positive result, you are pregnant. This is true no matter how faint the line, color, or sign is. If you get a positive result, you may want to call your doctor to talk about what comes next.
In
very rare cases, you can have a false-positive result. This means
you're not pregnant but the test says you are. You could have a
false-positive result if blood or protein is present in your urine. And
certain drugs, such as tranquilizers, anti-convulsants, or hypnotics, may also cause false-positive results.
If you get a negative result, you are likely not pregnant. However, you may still be pregnant if:
- The test is past its expiration date.
- You took the test the wrong way.
- You tested too soon.
- Your urine is too diluted because you consumed large amounts of fluid right before the test.
- You are taking certain medications, such as diuretics or antihistamines.
If you get a negative pregnancy test result, try retesting within about a week to double-check. Some home pregnancy tests suggest doing this regardless of your results.
What if you get two different results? Call your doctor. A blood test is a good idea to confirm results.
Taking Medicine During Pregnancy
There may come a time during your pregnancy
when you’re feeling under the weather and aren't sure if you can take
your regular over-the-counter (OTC) medication. Some medications are
safe to take during pregnancy. But others are not, or their effects on
your baby may not be known.
When
you meet with your doctor to confirm you're pregnant, ask what meds are
OK to take and what meds you need to find alternatives for. Your health care provider will weigh the risks and benefits to help you know what's safe.
Also, tell your doctor about any alternative medicines or supplements you take, even if the label says "natural." And if you get any new prescriptions while you're pregnant, make sure the people who prescribe them know that you're pregnant.
What Medications Are Safe to Take During Pregnancy?
Prenatal vitamins are safe and important to take when you're pregnant. Ask your health care provider about the safety of taking other vitamins, herbal remedies, and supplements. Most herbal preparations and supplements have not been proven to be safe during pregnancy.
Generally, you should not take any OTC medication while pregnant unless it is necessary.
The
following medications and home remedies have no known harmful effects
during pregnancy when taken according to the package directions. Contact
your doctor for additional information on their safety or for
medications not listed here.
Safe Medications to Take During Pregnancy*
Check with your doctor before taking these in the first trimester.
- Tylenol (acetaminophen)
- Saline nasal drops or spray
- Warm salt/water gargle
Check with your doctor before taking any other medications, especially in the first trimester.
First Aid Ointment
- Bacitracin
- J&J First-Aid Cream
- Neosporin
- Polysporin
- Benadryl cream
- Caladryl lotion or cream
- Hydrocortisone cream or ointment
- Oatmeal bath (Aveeno)
*Note: No drug can be considered 100% safe to use during pregnancy.
What Alternative Therapies Are Considered Safe During Pregnancy?
Some
alternative therapies have been shown to be safe and effective for
pregnant women to relieve some of the uncomfortable side effects of
pregnancy. Talk it over with your doctor first before using any of them.
And remember, “Natural” doesn’t always equal “safe” when you’re
pregnant.
Nausea in early pregnancy:Acupuncture, acupressure, ginger root (250 milligram capsules 4 times a day), and vitamin B6 (pyridoxine, 25 milligrams two or three times a day) work well. Sipping the thick syrup from inside a can of peaches, pears, mixed fruits, pineapples, or orange slices may also help.
Backache: Chiropractic manipulation holds the best track record. Another option is massage but it is important to make sure your massage therapist is adequately trained in pre-natal massage.
Turning a breech baby: Exercise and hypnosis may help.
Pain relief in labor:
Epidurals are most effective, but immersion in a warm bath can also
relieve tension. Relaxation and breathing techniques, emotional support,
and self-hypnosis are widely used in labor. Acupuncture can also work for some women.
What Alternative Therapies Should Be Avoided During Pregnancy?
The following substances in concentrated formulation (not as a spice in cooking) may harm your baby. Some are thought to cause birth defects and encourage early labor.
Avoid these oral supplements: Arbor vitae, beth root, black cohosh, blue cohosh, cascara, chaste tree berry, Chinese angelica (dong quai), cinchona, cotton root bark, feverfew, ginseng, golden seal, juniper, kava kava, licorice, meadow saffron, pennyroyal, poke root, rue, sage, St. John's wort, senna, slippery root, tansy, white peony, wormwood, yarrow, yellow dock, and vitamin A (large doses can cause birth defects).
Avoid these aromatherapy essential oils: Calamus, mugwort, pennyroyal, sage, wintergreen, basil, hyssop, myrrh, marjoram, and thyme.
When in doubt about any medication, supplement, or therapy, ask your health care provider before taking or using it.
NUTRITION AND FITNESS:
Eating Right When Pregnant
Good nutrition during pregnancy,
and enough of it, is very important for your baby to grow and develop.
You should consume about 300 more calories per day than you did before
you became pregnant.
Although nausea and vomiting during the first few months of pregnancy can make this difficult, try to eat a well-balanced diet and take prenatal vitamins. Here are some recommendations to keep you and your baby healthy.
Goals for Healthy Eating When Pregnant
- Eat a variety of foods to get all the nutrients you need. Recommended daily servings include 6-11 servings of breads and grains, two to four servings of fruit, four or more servings of vegetables, four servings of dairy products, and three servings of protein sources (meat, poultry, fish, eggs or nuts). Use fats and sweets sparingly.
- Choose foods high in fiber that are enriched, such as whole-grain breads, cereals, pasta and rice, as well as fruits and vegetables.
- Make sure you are getting enough vitamins and minerals in your daily diet while pregnant. You should take a prenatal vitamin supplement to make sure you are consistently getting enough vitamins and minerals every day. Your doctor can recommend an over-the-counter brand or prescribe a prenatal vitamin for you.
- Eat and drink at least four servings of dairy products and calcium-rich foods a day to help ensure that you are getting 1000-1300 mg of calcium in your daily diet during pregnancy.
- Eat at least three servings of iron-rich foods, such as lean meats, spinach, beans, and breakfast cereals each day to ensure you are getting 27 mg of iron daily.
- While you're pregnant, you will need 250 micrograms of iodine a day to help ensure your baby's brain and nervous system development. Choose from a variety of dairy products -- milk, cheese (especially cottage cheese), yogurt -- as well as baked potatoes, cooked navy beans, and limited amounts -- 8 to 12 oz per week -- of seafood such as cod, salmon, and shrimp.
- Choose at least one good source of vitamin C every day, such as oranges, grapefruits, strawberries, honeydew, papaya, broccoli, cauliflower, Brussels sprouts, green peppers, tomatoes, and mustard greens. Pregnant women need 70 mg of vitamin C a day.
- Choose at least one good source of folic acid every day, like dark green leafy vegetables, veal, and legumes (lima beans, black beans, black-eyed peas and chickpeas). Every pregnant woman needs at least 0.4 mg of folic acid per day to help prevent neural tube defects such as spina bifida.
- Choose at least one source of vitamin A every other day. Sources of vitamin A include carrots, pumpkins, sweet potatoes, spinach, water squash, turnip greens, beet greens, apricots, and cantaloupe.
Foods to Avoid When Pregnant
- Avoid alcohol during pregnancy. Alcohol has been linked to premature delivery, mental retardation, birth defects, and low birthweight babies.
- Limit caffeine to no more than 300 mg per day. The caffeine content in various drinks depends on the beans or leaves used and how it was prepared. An 8-ounce cup of coffee has about 150 mg of caffeine on average while black tea has typically about 80 mg. A 12-ounce glass of caffeinated soda contains anywhere from 30-60 mg of caffeine. Remember, chocolate (especially dark chocolate) contains caffeine -- sometimes a significant amount.
- The use of saccharin is strongly discouraged during pregnancy, because it can cross the placenta and may remain in fetal tissues. But, the use of other non-nutritive or artificial sweeteners approved by the FDA is acceptable during pregnancy. These FDA-approved sweeteners include aspartame (Equal or NutraSweet), acesulfame-K (Sunett), and sucralose (Splenda). These sweeteners are considered safe in moderation, so talk with your health care provider about how much non-nutritive sweetener is acceptable during pregnancy.
- Decrease the total amount of fat you eat to 30% or less of your total daily calories. For a person eating 2000 calories a day, this would be 65 grams of fat or less per day.
- Limit cholesterol intake to 300 mg or less per day.
- Do not eat shark, swordfish, king mackerel, or tilefish (also called white snapper), because they contain high levels of mercury.
- Avoid soft cheeses such as feta, Brie, Camembert, blue-veined, and Mexican-style cheese. These cheeses are often unpasteurized and may cause Listeria infection. There’s no need to avoid hard cheese, processed
- cheese, cream cheese, cottage cheese, or yogurt.
- Avoid raw fish, especially shellfish like oysters and clams.
What to Eat When Pregnant and Don't Feel Well
During pregnancy you may have morning sickness, diarrhea, or constipation. You may find it hard to keep foods down, or you may feel too sick to even eat at all. Here are some suggestions:
- Morning Sickness: Eat crackers, cereal, or pretzels before getting out of bed; eat small, frequent meals throughout the day; avoid fatty, fried, spicy, and greasy foods.
- Constipation: Eat more fresh fruit and vegetables. Also, drink 6 to 8 glasses of water a day.
- Diarrhea: Eat more foods that contain pectin and gums (two types of dietary fiber) to help absorb excess water. Examples of these foods are applesauce, bananas, white rice, oatmeal, and refined wheat bread.
- Heartburn: Eat small, frequent meals throughout the day; try drinking milk before eating; and limit caffeinated foods and beverages, citric beverages, and spicy foods.
Can I Diet While Pregnant?
No. Do not diet or try to lose weight during pregnancy -- both you and your baby need the proper nutrients in order to be healthy. Keep in mind that you will lose some weight the first week your baby is born.Can I Eat a "Low Carb" Diet When Pregnant?
Low-carbohydrate diets, such as Atkins and the South Beach Diet, are very popular. There have been no studies of the effects of a low-carb diet on pregnancy, so its effect on the fetus, if any, are unknown. While you are pregnant, you should eat a balanced diet, from all of the food groups.Can I Maintain My Vegetarian Diet When Pregnant?
Just because you are pregnant doesn't mean you have to diverge from your vegetarian diet. Your baby can receive all the nutrition he or she needs to grow and develop while you follow a vegetarian diet, if you make sure you eat a wide variety of healthy foods that provide enough protein and calories for you and your baby.Depending on the type of vegetarian meal plan you follow, you may need to adjust your eating habits to ensure that you and your baby are receiving adequate nutrition (you should consume about 300 more calories than you did before you became pregnant).Why Do I Need More Calcium When Pregnant?
Calcium is a nutrient needed in the body to build strong teeth and bones. Calcium also allows blood to clot normally, muscles and nerves to function properly, and the heart to beat normally. Most of the calcium in your body is found inside your bones.Your growing baby needs a considerable amount of calcium to develop. If you do not consume enough calcium to sustain the needs of your developing baby, your body will take calcium from your bones, decreasing your bone mass and putting you at risk for osteoporosis. Osteoporosis causes dramatic thinning of the bone, resulting in weak, brittle bones that can easily be broken.Pregnancy is a critical time for a woman to consume more calcium. Even if no problems develop during pregnancy, an inadequate supply of calcium at this time can diminish bone strength and increase your risk for osteoporosis later in life.
- The U.S. Recommended Daily Allowance (USRDA) for calcium is 1000 mg per day for pregnant and breastfeeding women over age 18. The USRDA for teenage girls up to age 18 is 1300 mg of calcium per day.
- Eating and drinking at least four servings of dairy products and calcium-rich foods a day will help ensure that you are getting the appropriate amount of calcium in your daily diet.
- The best sources of calcium are dairy products, including milk, cheese, yogurt, cream soups, and pudding. Calcium is also found in foods including green vegetables (broccoli, spinach, and greens), seafood, dried peas, and beans.
- Vitamin D will help your body use calcium. Adequate amounts of vitamin D can be obtained through exposure to the sun and in fortified milk, eggs, and fish.
How Can I Get Enough Calcium If I'm Lactose Intolerant?
Lactose intolerance is the inability to digest lactose, the sugar found in milk. If you are lactose intolerant, you may have cramping, gas, or diarrhea when dairy products are consumed.
If you are lactose intolerant, you can still receive the calcium you need. Here are some suggestions:
- Use Lactaid Milk fortified with calcium. Talk to your dietitian about other lactose-reduced products.
- You may be able to tolerate certain milk products that contain less sugar including cheese, yogurt, and cottage cheese.
- Eat non-dairy calcium sources, including greens, broccoli, sardines, and tofu.
- Try consuming small amounts of milk with meals. Milk is better tolerated with food.
Should I Take a Calcium Supplement During Pregnancy?
If
you have trouble consuming enough calcium-rich foods in your daily meal
plan, talk to your doctor or dietitian about taking a calcium
supplement. The amount of calcium you will need from a supplement
depends on how much calcium you are consuming through food sources.
Calcium supplements and some antacids containing calcium, such as Tums, may complement an already healthy diet. Many multiple vitamin supplements contain little or no calcium; therefore, you will need an additional calcium supplement.
Why Do I Need More Iron During Pregnancy?
Iron is a mineral that makes up an important part of hemoglobin, the substance in blood
that carries oxygen throughout the body. Iron also carries oxygen in
muscles, helping them function properly. Iron helps increase your
resistance to stress and disease.
The body absorbs
iron more efficiently during pregnancy; therefore, it is important to
consume more iron while you are pregnant to ensure that you and your
baby are getting enough oxygen. Iron will also help you avoid symptoms
of tiredness, weakness, irritability, and depression.
Following a balanced diet and including foods high in iron can help ensure that you are consuming enough iron throughout your pregnancy. In addition, the following guidelines will help:
- The U.S. RDA for iron is 27 mg per day for pregnant women and 15 mg for breastfeeding women.
- Eating at least three servings of iron-rich foods a day will help ensure that you are getting 30 mg of iron in your daily diet. One of the best ways to get iron from your diet is to consume a highly fortified breakfast cereal such as Total, which has 18 mg of iron. Note that iron intake is not equal to iron absorption. Absorption of iron into the body is greatest with meat sources of iron such as liver.
- The best sources of iron include enriched grain products, lean meat, poultry, fish, and leafy green vegetables.
What Are Good Sources of Iron?
- Meat and Seafood: Lean beef, chicken, clams, crab, egg yolk, fish, lamb, liver, oysters, pork, sardines, shrimp, turkey, and veal.
- Vegetables: Black-eyed peas, broccoli, Brussels sprouts, collard and turnip greens, lima beans, sweet potatoes, and spinach.
- Legumes: Dry beans and peas, lentils, and soybeans.
- Fruits: All berries, apricots, dried fruits, including prunes, raisins and apricots, grapes, grapefruit, oranges, plums, prune juice, and watermelon.
- Breads and Cereals: Enriched rice and pasta, soft pretzel, and whole grain and enriched or fortified breads and cereals.
- Other Foods: Molasses, peanuts, pine nuts, pumpkin, or squash seeds.
Should I Take an Iron Supplement During Pregnancy?
Talk to your health care
provider about an iron supplement. The National Academy of Sciences
recommends that all pregnant women following a balanced diet take an
iron supplement providing 27 mg of iron during the second and third
trimesters of pregnancy (that's the amount in most prenatal vitamins).
Your doctor may increase this dose if you become anemic. Iron deficiencyanemia
is a condition in which the size and number of red blood cells are
reduced. This condition may result from inadequate intake of iron or
from blood loss.
Other Facts About Iron
- Vitamin C helps your body use iron. It is important to include sources of vitamin C along with foods containing iron and iron supplements.
- Caffeine can inhibit the absorption of iron. Try to consume iron supplements and foods high in iron at least one to three hours before or after drinking or eating foods containing caffeine.
- Iron is lost in cooking some foods. To retain iron, cook foods in a minimal amount of water and for the shortest possible time. Also, cooking in cast iron pots can add iron to foods.
- Constipation is a common side effect of taking iron supplements. To help relieve constipation, slowly increase the fiber in your diet by including whole grain breads, cereals, fruits, and vegetables. Drinking at least eight cups of fluids daily and increasing moderate exercise (as recommended by your doctor) can also help you avoid constipation.
Food Cravings During Pregnancy
Food cravings during pregnancy are normal. Although there is no widely accepted explanation for food cravings,
almost two-thirds of all pregnant women have them. If you develop a
sudden urge for a certain food, go ahead and indulge your craving if it
provides energy or an essential nutrient. But, if your craving persists
and prevents you from getting other essential nutrients in your diet,
try to create more of a balance in your daily diet during pregnancy.
During
pregnancy, your taste for certain foods may change. You may suddenly
dislike foods you were fond of before you became pregnant. In addition,
during pregnancy, some women feel strong urges to eat non-food items
such as ice, laundry starch, dirt, clay, chalk, ashes, or paint chips.
This is called pica, and it may be associated with an iron deficiency such as anemia. Do not give in to these non-food cravings -- they can be harmful to both you and your baby. Tell your health care provider if you have these non-food cravings.
If
you have any problems that prevent you from eating balanced meals and
gaining weight properly, ask your health care provider for advice.
Registered dietitians -- the nutrition experts -- are available to help
you maintain good nutrition throughout your pregnancy.
EXERCISE:
Maintaining a regular exercise routine throughout your pregnancy can help you stay healthy and feel your best. Regular exercise during pregnancy can improve your posture and decrease some common discomforts such as backaches and fatigue. There is evidence that physical activity may prevent gestational diabetes (diabetes that develops during pregnancy), relieve stress, and build more stamina needed for labor and delivery.
If
you were physically active before your pregnancy, you should be able to
continue your activity in moderation. Don't try to exercise at your
former level; instead, do what's most comfortable for you now. Low
impact aerobics are encouraged versus high impact.
The pregnant competitive athlete should be closely followed by an obstetrician.
If you have never exercised regularly before, you can safely begin an exercise program during pregnancy after consulting with your health care provider, but do not try a new, strenuous activity. Walking is considered safe to initiate when pregnant.
The
American College of Obstetrics and Gynecology recommends 30 minutes or
more of moderate exercise per day on most if not all days of the week,
unless you have a medical or pregnancy complication.
Who Should Not Exercise During Pregnancy?
If you have a medical problem, such as asthma, heart disease, or diabetes, exercise may not be advisable. Exercise may also be harmful if you have a pregnancy-related condition such as:
- Bleeding or spotting
- Low placenta
- Threatened or recurrent miscarriage
- Previous premature births or history of early labor
- Weak cervix
Talk with your health care provider before beginning an exercise program. Your health care provider can also give you personal exercise guidelines, based on your medical history.
What Exercises Are Safe During Pregnancy?
Most exercises are safe to perform during pregnancy, as long as you exercise with caution and do not overdo it.
The safest and most productive activities are swimming,
brisk walking, indoor stationary cycling, step or elliptical machines,
and low-impact aerobics (taught by a certified aerobics instructor).
These activities carry little risk of injury, benefit your entire body,
and can be continued until birth.
Tennis
and racquetball are generally safe activities, but changes in balance
during pregnancy may affect rapid movements. Other activities such as jogging
can be done in moderation, especially if you were doing them before
your pregnancy. You may want to choose exercises or activities that do
not require great balance or coordination, especially later in
pregnancy.
To learn strength and toning exercises that are safe to do during pregnancy, see Sample Exercises.
What Exercises Should Be Avoided During Pregnancy?
There are certain exercises and activities that can be harmful if performed during pregnancy. They include:
- Holding your breath during any activity.
- Activities where falling is likely (such as skiing and horseback riding).
- Contact sports such as softball, football, basketball, and volleyball.
- Any exercise that may cause even mild abdominal trauma such as activities that include jarring motions or rapid changes in direction.
- Activities that require extensive jumping, hopping, skipping, bouncing, or running.
- Deep knee bends, full sit-ups, double leg raises, and straight-leg toe touches.
- Bouncing while stretching.
- Waist-twisting movements while standing.
- Heavy exercise spurts followed by long periods of no activity.
- Exercise in hot, humid weather.
What Should a Pregnancy Exercise Program Consist Of?
For total fitness, a pregnancy exercise program should strengthen and condition your muscles.
Always begin by warming up for five minutes and stretching for five minutes. Include at least fifteen minutes of cardiovascular activity. Measure your heart rate
at times of peak activity. Follow aerobic activity with five to ten
minutes of gradually slower exercise that ends with gentle stretching.
Here are some basic exercise guidelines for pregnant women:
- Wear loose fitting, comfortable clothes as well as a good support bra.
- Choose shoes that are designed for the type of exercise you do. Proper shoes are your best protection against injury.
- Exercise on a flat, level surface to prevent injury.
- Consume enough calories to meet the needs of your pregnancy (300 more calories per day than before you were pregnant) as well as your exercise program.
- Finish eating at least one hour before exercising.
- Drink water before, during, and after your workout.
- After doing floor exercises, get up slowly and gradually to prevent dizziness.
- Never exercise to the point of exhaustion. If you cannot talk normally while exercising, you are probably over-exerting yourself and should slow down your activity.
What Pregnancy Changes May Affect Exercise?
Physical
changes during pregnancy create extra demands on your body. Keeping in
mind the changes listed below, remember that you need to listen to your
body and adjust your activities or exercise routine as necessary.
- Your developing baby and other internal changes require more oxygen and energy.
- Hormones produced during pregnancy cause the ligaments that support your joints to stretch, increasing the risk of injury.
- The extra weight and the uneven distribution of your weight shift your center of gravity. The extra weight also puts stress on joints and muscles in the lower back and pelvic area and makes it easier for you to lose your balance.
- Stop exercising and consult your health care provider if you:
- Feel chest pain.
- Have abdominal pain, pelvic pain, or persistent contractions.
- Have a headache.
- Notice an absence or decrease in fetal movement.
- Feel faint, dizzy, nauseous, or light-headed.
- Feel cold or clammy.
- Have vaginal bleeding.
- Have a sudden gush of fluid from the vagina or a trickle of fluid that leaks steadily.
- Notice an irregular or rapid heartbeat.
- Have sudden swelling in your ankles, hands, face, or calf pain.
- Are short of breath.
- Have difficulty walking.
- Have muscle weakness.
How Soon Can I Exercise After Delivery?
It is best to ask your health care provider how soon you can begin your exercise routine after delivering your baby.
Although
you may be eager to get in shape quickly, return to your pre-pregnancy
fitness routines gradually. Follow your health care provider's exercise
recommendations.
Most women can safely
perform a low-impact activity one to two weeks after a vaginal birth (or
three to four weeks after a cesarean birth). Do about half of your
normal floor exercises and don't try to overdo it.
WEIGHT GAIN:
Gain Weight Safely During Your Pregnancy
Eating a healthy, balanced diet will help your baby get the nutrients he or she needs and grow at a healthy rate. But how many extra calories do you really need?
Though you do need some extra calories, it's not necessary to ''eat for two.'' The average pregnant woman needs only about 300 healthy calories more a day than she did before she was pregnant. This will help her gain the right amount of weight during pregnancy.
Ask your health care provider how much weight you should gain. A woman who was average weightbefore getting pregnant should gain 25 to 35 pounds after becoming pregnant. Underweight women should gain 28 to 40 pounds. And overweight women may need to gain only 15 to 25 pounds during pregnancy.
In
general, you should gain about 2 to 4 pounds during the first three
months you're pregnant and 1 pound a week during the rest of your
pregnancy. If you are expecting twins you should gain 35 to 45 pounds
during your pregnancy. This would be an average of 1 ½ pounds per week
after the usual weight gain in the first three months.
It's
especially important to gain the right amount of weight when you're
expecting twins because your weight affects the babies' weight. And
because twins are often born before the due date, a higher birth weight is important for their health. When carrying twins, you may need between 3,000 and 3,500 calories a day.
Where Does the Extra Weight Go During Pregnancy?
- Baby: 8 pounds
- Placenta: 2-3 pounds
- Amniotic fluid: 2-3 pounds
- Breast tissue: 2-3 pounds
- Blood supply: 4 pounds
- Stored fat for delivery and breastfeeding: 5-9 pounds
- Larger uterus: 2-5 pounds
- Total: 25-35 pounds
Is It Safe to Lose Weight When Pregnant?
If a woman is very overweight
when she gets pregnant, her doctor may want her to lose weight. She
should only lose weight under her doctor's care. But in most cases,
women should not try to lose weight or diet during pregnancy.
How to Gain the Right Amount of Weight During Pregnancy
If your health care provider wants you to gain weight while you're pregnant, try these tips:
- Eat five to six small meals every day.
- Keep quick, easy snacks on hand, such as nuts, raisins, cheese and crackers, dried fruit, and ice cream or yogurt.
- Spread peanut butter on toast, crackers, apples, bananas, or celery. One tablespoon of creamy peanut butter gives you about 100 calories and 7 grams of protein.
- Add nonfat powdered milk to mashed potatoes, scrambled eggs, and hot cereal.
- Add extras to your meal, such as butter or margarine, cream cheese, gravy, sour cream, and cheese.
What if You Gain Too Much Weight During Pregnancy?
If you have gained more weight than your doctor recommended, talk to
your doctor about it. In most cases, you'll want to wait until after
delivery to lose weight.
Here are some tips to slow your weight gain:
- When eating fast food, choose lower-fat items such as broiled chicken breast sandwich with tomato and lettuce (no sauce or mayonnaise), side salad with low-fat dressing, plain bagels, or a plain baked potato. Avoid foods such as French fries, mozzarella sticks, or breaded chicken patties.
- Avoid whole milk products. You need at least four servings of milk products every day. However, using skim, 1%, or 2% milk will greatly reduce the amount of calories and fat you eat. Also, choose low-fat or fat-free cheese or yogurt.
- Limit sweet or sugary drinks. Sweetened drinks such as soft drinks, fruit punch, fruit drinks, iced tea, lemonade, or powdered drink mixes have lots of empty calories. Choose water, club soda, or mineral water to skip extra calories.
- Don't add salt to foods when cooking. Salt causes you to retain water.
- Limit sweets and high-calorie snacks. Cookies, candies, donuts, cakes, syrup, honey, and potato chips have a lot of calories and little nutrition. Try not to eat these foods every day. Instead, try fresh fruit, low-fat yogurt, angel food cake with strawberries, or pretzels as lower-calorie snack and dessert choices.
- Use fats in moderation. Fats include cooking oils, margarine, butter, gravy, sauces, mayonnaise, regular salad dressings, sauces, lard, sour cream, and cream cheese. Try lower-fat alternatives.
- Cook food the healthy way. Frying foods in oil or butter will add calories and fat. Baking, broiling, grilling, and boiling are healthier preparation methods.
- Exercise. Moderate exercise can help burn excess calories. Walking or swimming is usually safe for pregnant women. Ask your health care provider what exercise would be right for you before getting started.
FIRST TRIMESTER(THREE MONTHS) OF PREGNANCY:
First Trimester of Pregnancy
Having a baby
is one of the most joyous times in many women's lives. From
anticipating the day you'll bring your little one home, to picking a
name and nursery colors, the excitement is palpable.
But
no matter how well you plan for their arrival, you may not be fully
prepared for all of the changes your body will go through now. Knowing
what to expect will help you get ready for the months ahead.
What to Expect: Changes in Your Body
Pregnancy
is different for every woman. Some women glow with good health and
vitality during those first three months; others feel absolutely
miserable. Here are some of the changes you might experience, what they
mean, and which signs warrant a call to your doctor.
Bleeding. About 25% of pregnant women experience slight bleeding during their first trimester.
Early in the pregnancy, light spotting may be a sign that the
fertilized embryo has implanted in the uterus. However, if you have
significant bleeding, cramping, or sharp pain in your abdomen, call your doctor. These could be signs of a miscarriage or ectopic pregnancy (a pregnancy in which the embryo implants outside of the uterus).
Breast tenderness. Sore breasts are one of the earliest signs of pregnancy.
They're triggered by hormonal changes, which are preparing your milk
ducts to feed your baby, and will probably last through the first
trimester. Going up a bra size (or more) and wearing a support bra can
make you feel more comfortable; you can go back to the lacy bras after
your baby is finished nursing.
Constipation. During pregnancy, the muscle contractions that normally move food through your intestines slow down because of higher levels of the hormone progesterone. Add to that the extra iron you're getting from your prenatal vitamin, and the result is uncomfortable constipation
and gas that can keep you feeling bloated throughout your pregnancy.
Increase your fiber intake and drink extra fluids to keep things moving
more smoothly. Physical activity can also help.
If your constipation is really bothering you, talk to your doctor about what mild laxative or stool softeners are safe to use during pregnancy.
Discharge. It's normal to see a thin, milky white
discharge (called leukorrhea) early in your pregnancy. You can wear a
panty liner if it makes you feel more comfortable, but don't use a
tampon because it can introduce germs into the vagina. If the discharge is foul-smelling, green, or yellow, or if there's a lot of clear discharge, call your doctor.
Fatigue. Your body is working hard to support a growing fetus,
which can wear you out more easily than usual. Take naps or rest when
you need to throughout the day. Also make sure you're getting enough
iron (too little can lead to anemia, which can cause excess fatigue).
Food cravings and aversions. Although you may not want a bowl of mint chip ice cream topped with dill pickles, as the old stereotype goes, your tastes can
change while you're pregnant. More than 60% of pregnant women
experience food cravings, and more than half have food aversions,
according to research. Giving in to cravings from time to time is OK,
provided you are generally eating healthy, low-calorie foods. The
exception is pica
-- a craving for non-foods like clay, dirt, and laundry starch, which
can be dangerous for you and your baby. If you experience this kind of
craving, report it to your doctor right away.
Frequent urination. Your baby is still pretty small, but your uterus is growing and it's putting pressure on your bladder.
As a result, you may feel like you constantly have to go to the
bathroom. Don't stop drinking fluids -- your body needs them -- but do
cut down on caffeine (which stimulates the bladder), especially before bedtime. When nature calls, answer it as soon as you can. Don't hold it in.
Heartburn.
During pregnancy, your body produces more of the progesterone hormone
which relaxes smooth muscles -- including the ring of muscle in your
lower esophagus that normally keeps food and acids down in your stomach. This muscle relaxation can lead to acid reflux, otherwise known as heartburn. To avoid the burn,
eat frequent, smaller meals throughout the day; don't lie down right
after eating; and avoid greasy, spicy, and acidic foods (like citrus
fruits). You can also try raising your pillows when you sleep.
Mood swings. Increased fatigue
and changing hormones can put you on an emotional roller coaster that
makes you feel alternately elated and miserable, cranky and terrified.
It's OK to cry, but if you're feeling overwhelmed, try to find an
understanding ear -- if not from your partner, then from a friend or
family member.
Morning sickness. Nausea is one of the most universal pregnancy symptoms,
affecting up to 85% of pregnant women. It's the result of hormone
changes in the body, and it can last through the entire first trimester.
For some pregnant women, nausea is mild; others can't start their day
without vomiting. Nausea is usually worst in the morning (hence the name, "morning sickness"). To calm your nausea, try eating small, bland, or high-protein
snacks (crackers, meat, or cheese) and sipping water, clear fruit juice
(apple juice), or ginger ale. You may want to do even do this before
getting out of bed. Avoid any foods that make you sick to your stomach. Nausea itself isn't anything to worry about, but if it persists or is severe, it can affect the amount of nutrition getting to your baby, so call your doctor if you can't stop vomiting or can't keep down any food.
Weight gain.
Pregnancy is one of the few times in a woman's life when weight gain is
considered a good thing, but don't overdo it. During the first
trimester, you should gain about 3 to 6 pounds (your doctor may
recommend that you adjust your weight gain up or down if you started
your pregnancy underweight or overweight).
Although you're carrying an extra person, don't go by the adage of
"eating for two." You only need about an extra 150 calories a day during
your first trimester. Get those calories the healthy way, by adding
extra fruits and vegetables, milk, whole-grain bread, and lean meat to your diet.
Red Flag Symptoms
Any
of these symptoms could be a sign that something is seriously wrong
with your pregnancy. Don't wait for your prenatal visit to talk about
it. Call your doctor right away if you experience:
- Severe abdominal pain.
- Significant bleeding.
- Severe dizziness.
- Rapid weight gain or too little weight gain.
Your Pregnancy Week by Week: Weeks 1-4
FIRST MONTH:
If
you are newly pregnant or trying to conceive, you have many questions
about what to expect. How will your body change? What's happening inside
you? Our week-by-week guide will help you through your nine months of pregnancy
so you can be a smarter, more confident, more prepared mom-to-be. Each
week offers information about your body and the baby's as well as
helpful advice you can use throughout your pregnancy. Let's start with a
peek inside the womb.
Weeks 1 and 2
Baby: Your baby is still just a glimmer in your eye. It’s difficult to know exactly when conception occurred, so doctors calculate your due date
from the beginning of your last menstrual cycle. That’s right -- for
calculation purposes, you’re “pregnant” before you even conceive!
Mom-to-be: At
the beginning of your period, about 20 eggs called ova occupy
fluid-filled sacs called follicles. If you typically have your period
every 28 days, then about 14 days later, you ovulate: One of these
follicles releases an egg, and it travels down your fallopian tube where
it awaits fertilization. This time -- 14 days after your period started
and a day or so longer -- is when you're the most fertile. If you want
to get pregnant, this is the best time to try. Once the egg is fertilized, it moves into the uterus.
Don't be disappointed if you don't get pregnant the first time. Each month, women have a 25% chance of getting pregnant, so you may need to try more than once.
Tip for the Week: Make
sure you've scheduled a preconception visit with your ob-gyn to
determine risks of genetic diseases and environmental hazards as well as
learn about necessary lifestyle changes to ensure a healthy pregnancy
and baby. Most important, make sure you've started taking 0.4
milligrams, or 400 micrograms, of folic acid a day. Folic acid taken a few months before conception has been shown to dramatically reduce such neural tube defects as spina bifida.
Week 3
Baby: Congratulations! If your egg and your partner's sperm
have joined successfully, your embryo is really there, although it's
very small -- about the size of the head of a pin. It doesn't look like a
fetus
or baby; it's just a group of about 100 cells multiplying and growing
rapidly. The outer layer of cells will become the placenta, and the
inner layer will become the embryo.
Mom-to-be: You won't notice any changes in your body at this point. Remember, you haven't even missed your period yet.
Tip for the Week: Can't wait to find out? Take a home pregnancy test. They're about as reliable as a urine test or blood
test done in the doctor's office -- and you get results immediately. To
ensure accuracy, read the directions carefully and make sure all the
supplies you use are clean.
Week 4
Baby: Now that your egg is fertilized, it burrows into the lining of your uterus. This is called implantation.
Mom-to-be: You're
probably expecting your period this week, and if it doesn't occur, it
might be one of the first signs that you're pregnant. You may also
notice light spotting as the embryo implants itself in your uterus. You
might not feel any different yet, but the amniotic cavity, which will be
filled with fluid, and the placenta, which will bring oxygen and nutrients to nourish your baby, are forming in your uterus.
Tip for the Week: Try
to eat healthfully, which means choosing a variety of foods from
recommended food groups and drinking at least six to eight 8-ounce
glasses of water a day. But you don't really need to "eat for two"; you
only need an extra 300 calories per day while you're pregnant. And don't
worry if your food intake drops in the beginning because of morning sickness. If you've been eating right already, your baby will get what it needs.
What's Happening Inside You?
The
fertilized egg grows, and a water-tight sac forms around it, gradually
filling with fluid. This is called the amniotic sac, and it helps
cushion the growing embryo.
The placenta also develops. It is a round, flat organ that transfers nutrients from you to the baby and transfers baby’s wastes.
A primitive face takes form with large dark circles for eyes. The mouth, lower jaw, and throat are developing. Blood cells are taking shape, and circulation will begin.
By the end of the first month, your baby is about 1/4 inch long --smaller than a grain of rice.
Your Pregnancy Week by Week: Weeks 5-8
SECOND MONTH:
Week 5
Baby: Your baby is still tiny, but its heart, brain,
spinal cord, muscle, and bones are beginning to develop. The placenta,
which nourishes your baby, and the amniotic sac, which provides a warm
and safe environment where your baby can move easily, are still forming,
too. The umbilical cord forms and connects your baby to your blood supply.
Mom-to-be: You might suspect by now that you're pregnant. You may also notice some early symptoms of pregnancy:
- Feeling nauseous (called morning sickness, although it can happen at any time of day or night)
- Tingling or soreness in your breasts and darkening of your nipples
- Needing to pee more often
- Feeling more tired than usual
Tip of the Week:
You'll want to schedule a visit to your ob-gyn as soon as you suspect
you're pregnant. Starting prenatal care early and keeping up with your
appointments is a large step toward having a healthy pregnancy and a healthy baby.
Week 6
Baby: Your baby is shaped like a tadpole, and it's about the size of a BB pellet. The eyes and limb buds are forming. During an ultrasound,
your doctor may be able to hear a heartbeat. Between days 17 and 56 is a
vulnerable time, because that's when the baby is most susceptible to
anything that can affect normal growth.
Mom-to-be: You may have gained a few pounds by now. Or if you're having morning sickness you may have lost weight
-- that's normal, too. You may start noticing some changes in your
body: clothes getting a little tighter around your waist, fuller legs
and breasts. With a pelvic exam, your doctor will notice a change in the size of your uterus.
Tip of the Week: Follow good prenatal habits each day, like eating healthfully and taking prenatal vitamins. If you haven't already, stop smoking and drinking alcohol.
Week 7
Baby: Your baby is growing. Limb buds appear that will grow into hands and feet. Many parts continue to develop: heart, lungs, intestines, appendix, brain, spinal cord, nostrils, mouth, and eyes.
Mom-to-be:
You're still not "showing," but by now you're really feeling the
changes in your body. You may still have morning sickness, and your
breasts probably still feel tingly and tender.
Tip of the Week: Never let your stomach
get completely empty -- that will help you from feeling queasy. Keep
snacks on hand around the clock, and eat lots of little meals rather
than three big ones. To prevent a drop in blood sugar, eat some protein, like adding cheese to crackers.
Week 8
Baby: Your
baby is now about in its sixth week of development. It's a big week for
growth. Eyelid folds and ears are forming. Your baby develops little
webbed fingers and toes and can even swim around in your womb.
Mom-to-be: Your blood
volume is increasing, and your heart is pumping 50% more blood per
minute for your baby. Common symptoms for this week are moodiness and
queasiness from certain smells.
Tip of the Week:
Wear a supportive bra. Good breast support during pregnancy will help
you feel more comfortable and prevent future sagging. Exercises to keep
your chest muscles toned can be useful, too.
What's Happening Inside You?
Your baby's facial features continue to develop. Each ear begins as a little fold of skin at the side of the head. Tiny buds that eventually grow into arms and legs are forming. So are fingers and toes.
The neural tube (brain, spinal cord, and other nerve tissue) is well formed. The digestive tract and sensory organs begin to develop. Bone starts to replace cartilage.
THIRD MONTH:
9 Weeks Pregnant
Baby: Your baby is about the size of a peanut. The head is more erect, and the neck is more developed. During an ultrasound, you might see how your baby moves, even though you can't feel it yet.
Mom-to-be:
Your uterus is continuing to grow, and you may notice your waistline
thickening. Unless you tell people your special news, however, your pregnancy still won't be noticeable to others. You shouldn't have gained much weight yet, especially if you're having food aversions, cravings, heartburn, indigestion, nausea, or bloating.
Tip of the Week: Eat plenty of foods that contain calcium, such as cheeses, sardines, and broccoli. Your baby needs it, and so do you.
10 Weeks Pregnant
Baby: Your baby is still small but looks and acts like a baby. Arms and legs are longer and can bend at the elbows and knees.
Mom-to-be:
Once the size of your fist, your uterus is now the size of a
grapefruit. You still probably don't show much, but you may feel more
comfortable in looser clothes. You may continue to feel tired and moody,
but take heart: These symptoms shouldn't last too much longer.
Tip of the Week: Start shopping for maternity bras. You'll need one pretty soon. You can go ahead and get nursing bras if you're planning to breastfeed.
11 Weeks Pregnant
Baby:
It's another big growth week. When your doctor uses a Doppler
stethoscope now, she can hear the rapid "swooshing" noises of the
heartbeat. Your baby's genitals are developing, but the sex can't be determined yet.
Mom-to-be: Pregnancy hormones show their good and bad effects. You may notice that your hair, fingernails, and toenails are growing faster. But you may also notice oily skin and acne.
Tip of the Week:
Schedule a dentist appointment. See your dentist at least once in these
nine months. Brush and floss daily, and take your prenatal vitamin for calcium to keep your teeth strong. Your gums may bleed more because of pregnancy hormones and increased blood volume. If they do, use a soft toothbrush.
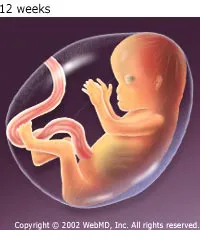
12 Weeks Pregnant
Baby: All parts of your baby are developing, from tooth buds to toenails.
Your baby will keep developing and getting larger and stronger for the
rest of your pregnancy. By the end of this week, the chance of miscarriage drops considerably.
Mom-to-be:
You'll feel more energetic for the next few weeks. The typical weight
gain by now is from 1.5 to 5 pounds. Fathers-to-be might also experience
pregnancy symptoms, called couvade, or "hatching," during the third month and at delivery, including nausea, abdominal pain, appetite changes, and weight gain.
Tip of the Week: Try not to fret about stretch marks. Most women get them on the breasts, abdomen,
hips, or buttocks sometime during pregnancy. They won't go away, but
they usually fade after pregnancy. Despite claims from manufacturers,
creams and oils don't minimize them. How much they show depends on your
skin's natural elasticity.
What's Happening Inside You?
By
the end of the third month, your baby is fully formed, with arms,
hands, fingers, feet, and toes. Little hands can open and close.
Fingernails and toenails are beginning to develop, and the external ears
are formed. Teeth are starting to form. Your baby's reproductive organs also develop, but the baby's sex is difficult to distinguish on ultrasound. The circulatory and urinary systems are working, and the liver produces bile.
Your Guide to Prenatal Testing
When you’re pregnant,
prenatal tests give you information about your health and your baby’s.
They help detect any problems that could affect him, like birth defects or genetic diseases. The results can help you make the best health care decisions before and after your child is born.
Prenatal
tests are helpful, but it’s important to know how to interpret what
they find. A positive test result doesn’t always mean your baby will be
born with a disorder. You’ll want to talk with your doctor, midwife, or other health care provider about what the tests mean and what you should do once you have the results.
Doctors
recommend some prenatal tests for all pregnant women. Only some women
will need other screening tests to check for certain genetic problems.
Routine Prenatal Tests
There are different prenatal tests you can get in your first, second, and third trimester. Some check your health, and others get information about your baby.
Throughout your pregnancy, you’ll get routine exams to make sure you’re healthy. Your health care provider will check samples of your blood and urine for certain conditions, including:
- HIV and other sexually transmitted diseases
- Anemia
- Diabetes
- Hepatitis B
- Preeclampsia, a type of high blood pressure
She’ll also check your blood type and whether your blood cells have a protein called the Rh factor. You may also get:
- Pap smear
- Group B Strep screening. Your doctor will swab the skin in and around your vagina to check for this type of bacteria. This usually happens in the last month before you give birth.
- Ultrasound. This technology uses sound waves to make pictures of your baby and your organs. If your pregnancy is normal, you’ll have it twice, once near the beginning to see how far along you are, and the second time around 18-20 weeks to check your baby’s growth and make sure his organs are developing properly.
Prenatal Genetic Tests
Doctors
also can use prenatal tests to look for signs that your baby is at risk
for certain genetic disorders or birth defects. You don’t have to have
these tests, but your doctor may suggest some to make sure your baby is
healthy.
Prenatal Genetic Tests continued...
They’re especially important for women who have a higher risk of having a baby with a birth defect or a genetic problem.This is you if you:
- Are over age 35
- Have had a premature baby or a baby with a birth defect before
- Have a genetic disorder or one that runs in your family or the other parent’s family
- Have a medical condition like diabetes, high blood pressure, a seizure disorder, or an autoimmune disorder such as lupus
- Have had miscarriages or stillborn babies in the past
- Have had gestational diabetes or preeclampsia when you were pregnant before
Some
prenatal genetic tests are screening tests. They tell you if your baby
has a higher risk of having a certain disorder or disease, but they
can’t tell you for certain that he’ll be born with it. Other
“diagnostic” tests will give you a more definite answer. Usually, you’ll
get this kind after you have a positive result on a screening test.
To start, your doctor may want to test you and the child’s other parent for the genes that cause certain genetic diseases, like cystic fibrosis, Tay-Sachs disease, sickle cell disease,
and others. If both of you have a gene for one of these diseases in
your DNA, you could pass it on to your baby, even if you don't have the
disease itself. The exam is called a carrier test.
Your doctor can use one or more different screening tests to check your baby for a genetic problem, including:
Ultrasound.
You’ll already have one of these early in your pregnancy to make sure
everything is going well. But if you have a high-risk pregnancy, you’ll
need this exam more often. Around 11-14 weeks, doctors can use it to
look at the back of your baby’s neck. Folds or thick skin there could
mean a higher risk of Down syndrome. Your doctor also may take a sample of your blood at the same time.
Integrated Screening.
There are two phases to this test. In the first part, doctors combine
the results of the ultrasound looking at your baby’s neck and the blood
tests you got at 11-14 weeks. Then, they’ll take a second blood sample
between 16-18 weeks. The results measure your baby’s risk for Down
syndrome and spina bifida, a spinal cord and brain disorder.
Sequential Screen. This is similar to integrated
screening, but your doctor reviews the results with you right after the
first phase at 11-14 weeks. It’s not as accurate as the longer test, but
it lets you know your baby’s risk earlier. If the screening finds there
may be a problem, your doctor will use more tests to find out for sure.
If it doesn’t find a risk, you’ll most likely get the second blood test
at 16-18 weeks to be safe.
Triple or quadruple screening test. Doctors
check your blood for hormones and proteins that come from your baby or
your placenta, the organ that brings him oxygen and nutrients.
The test can look for three different substances (triple screening) or
four (quadruple screening). Certain amounts of these mean your baby has a
higher chance of having a birth defect or a genetic disease. This test
happens in the second trimester, usually at 15 to 20 weeks.
Cell-free fetal DNA testing. Doctors use this test to find your baby’s DNA in your blood and check it for Down syndrome and two other genetic conditions, trisomy 18
and trisomy 13. You can have this done after 10 weeks of your
pregnancy. Doctors don’t recommend it for every woman, usually only
those who have a high-risk pregnancy. It’s not available everywhere, and
some health insurance policies don’t cover it. Talk to your doctor
about whether you need this test.
Other Tests
If you get a positive result on a screening, your doctor can use other tests to look for a problem.
Amniocentesis. Using
a thin needle in your belly, your doctor will take a sample of the
fluid that surrounds your baby and check it for genetic disorders or
birth defects. The procedure does carry some risk. About 1 in 300 to 500
women will miscarry because of amniocentesis. Your doctor can tell you if it’s important for you to have this.
Chorionic villus sampling (CVS). Doctors take a small piece of your placenta by putting a needle through your belly or a small tube up your vagina.
They test the sample for Down syndrome and other genetic conditions.
Only some high-risk women will need this test, usually if a screening
found a risk of a birth defect. The procedure will tell you for sure if
there’s a problem, but it also comes with a risk of miscarriage that’s
similar to amniocentesis. Talk to your doctor about whether you should
have CVS.
What Do I Do Once I Have the Results?
Prenatal
test results can help you make important health care decisions. But
it’s important to remember that many of them tell you it’s possible, but
not certain, that your baby will be born with a disorder. No test is
100% accurate.
Talk to your doctor about the results
you get and what they mean. A genetics counselor can also help you
decide what to do after a positive result and what life will be like for
your child if he has a disorder.
Questions for Your Doctor
If your doctor recommends prenatal testing, consider asking:
- Why do I need these tests?
- What will the results tell me? What will they not show?
- What happens if I don't get the test?
- What will I do with the results?
- How accurate are the tests?
- What are the risks?
- How long will it take to get the results?
- What does it feel like?
- How much do they cost?
- Will my insurance cover them?
- Will anyone else (like my insurance company) have access to the results, especially of genetic tests?
- What will the results mean for my family?
- Can I decide not to get the results even if the test has already been done?
- Where do I get the tests done?
First trimester tests during pregnancy
Here are some tests you may undergo during the first trimester of your pregnancy:
Blood tests: During one of your initial examinations, your doctor or midwife will identify your blood type and Rh (rhesus) factor, screen for anemia, check for immunity to rubella (German measles), and test for hepatitis B, syphilis, and HIV and other sexually transmitted diseases.
Depending
on racial, ethnic, or family background, you may be offered tests and
genetic counseling to assess risks for diseases such as Tay-Sachs, cystic fibrosis, and sickle cell anemia
(if these weren't done at a preconception visit). Tests for exposure to
diseases such as toxoplasmosis and varicella (the virus that causes
chickenpox) may also be done if needed. Your health care provider may also want to check your levels of hCG, a hormone secreted by the placenta, and/or progesterone, a hormone that helps maintain the pregnancy.
Urine tests: You will also be asked early on for a urine sample so that your doctor or midwife can look for signs of kidney infection
and, if necessary, to confirm your pregnancy by measuring the hCG
level. (A blood hCG test to confirm pregnancy may be used instead.)
Urine samples will then be collected regularly to detect glucose (a sign
of diabetes) and albumin (a protein that may indicate preeclampsia, pregnancy-induced high blood pressure).
In
the later part of the first trimester you will be offered genetic
testing. You first have to decide if you want any genetic testing at
all. Some people feel like these tests may cause them undue stress and
they prefer to make sure the baby is genetically normal after the baby
is born. Some people want to go ahead and do all the testing they can
realizing that these tests sometimes are not 100% accurate. Talk with
your doctor about the pros and the cons before proceeding to see if
genetic testing is right for you and your pregnancy. There are different
genetic testing options that involve blood tests alone or with an ultrasound that involve no risk to the fetus.
If these non invasive tests are abnormal, then further testing will be
offered to you. At that point, you can decide if you want to do those
tests or not.
One first semester genetic test combines a blood test with an ultrasound to screen for Down syndrome
may be available between 11 and 14 weeks of pregnancy. The results of a
blood test that measures hCG and/or PAPP-A (pregnancy-associated plasma
protein A) in maternal blood are used with an ultrasound measurement of
the skin at the back of the fetus’
neck (called nuchal translucency). The procedure may be able to pick up
a substantial portion of Down syndrome cases and other genetic
conditions. However, as with all screening methods, a more invasive
diagnostic technique like CVS is used if results are positive.
Non-Invasive Prenatal Testing
(NIPT) screening: This cell-free fetal DNA test can be done as early as
after 10 weeks of pregnancy. The test uses a blood sample to measure
the relative amount of free fetal DNA in a mother's blood. It's thought
that the test can detect 99% of all Down syndrome pregnancies. It also
tests for some other chromosomal abnormalities.
Chorionic villus sampling
(CVS): If you're 35 or older, have a family history of certain
diseases, or have had a positive result on non-invasive genetic tests,
you will be offered this optional, invasive test usually between 10 and
12 weeks of pregnancy. CVS can detect many genetic defects, such as Down
syndrome, sickle cell anemia, cystic fibrosis, hemophilia, and muscular dystrophy. The procedure involves either threading a tiny catheter through your cervix or inserting a needle into your abdomen to obtain a tissue sample from the placenta. The procedure carries a 1% risk of inducing miscarriage and is about 98% accurate in ruling out certain chromosomal birth defects. But, in contrast to amniocentesis, it does not help in detecting neural tube disorders, such as spina bifida and anencephaly, or abdominal wall defects.
Be
sure to discuss all of your testing options with your doctor so that
together you can decide on the ones that will be best for you.
3D and 4D Ultrasounds
Who Gets the Test?
3D and 4D ultrasounds are optional. They're not standard prenatal tests. Doctors often give them as a courtesy to women who want them.
Not all doctors have access to 3D or 4D ultrasounds. Also, your insurance may not cover the cost.
What the Test Does
Like
regular ultrasounds, 3D and 4D ultrasounds use sound waves to create an
image of your baby in your womb. What's different is that 3D
ultrasounds create a three-dimensional image of your baby, while 4D
ultrasounds create a live video effect, like a movie -- you can watch
your baby smile or yawn.
Parents often want 3D and 4D
ultrasounds. They let you see your baby's face for the first time. Some
doctors like 3D and 4D ultrasounds because they can show certain birth defects, such as cleft palate, that might not show up on a standard ultrasound.
Studies
suggest that 3D and 4D ultrasounds are safe. Plus, the images can help
doctors spot a problem with your baby and make it easier for them to
explain it to you.
The concern comes with companies
that offer keepsake ultrasounds. Groups like the American Institute of
Ultrasound in Medicine and the American Congress of Obstetricians and
Gynecologists caution that too much exposure to any ultrasound may not
be good for your baby. Getting an ultrasound just to see your baby's
face may not be a good idea -- especially at an ultrasound center in a
local mall or office building that may or may not employ highly skilled
technicians.
Talk about the pros and cons with your doctor.
How the Test Is Done
For an abdominal ultrasound,
you'll lie down and a technician will put a certain gel on your belly.
This helps carry the sound waves. Then the technician will hold a probe
against your belly and move it around to get an image.
What to Know About Test Results
Afterward, you may get photos or a copy of a 4D movie to take home. Your doctor will tell you if anything seems unusual.
Keep
in mind that 3D and 4D ultrasounds are not typically used to diagnose
problems with your baby. Also, getting an ultrasound at a commercial
center is not a substitute for medical care. The people working there
may not be qualified to diagnose or rule out problems.
How Often the Test Is Done During Your Pregnancy
3D and 4D ultrasounds are optional.
Other Names for This Test
Sonogram, abdominal ultrasound, abdominal sonogram
Tests Similar to This One
Ultrasound (standard), level II ultrasound
HEALTH CONCERN IN FIRST TREMESTER:
What is a high-risk pregnancy?
Your pregnancy is
called high-risk if you or your baby has an increased chance of a health
problem. Many things can put you at high risk. Being called "high-risk" may
sound scary. But it's just a way for doctors to make sure that you get special
attention during your pregnancy. Your doctor will watch you closely during your
pregnancy to find any problems early.
The conditions listed below
put you and your baby at a higher risk for problems, such as slowed growth for
the baby,
preterm labor,
preeclampsia, and problems with the
placenta. But it's important to remember that being at
high risk doesn't mean that you or your baby will have problems.
Your health plan may have its own list of what makes a pregnancy
high-risk. In general, your pregnancy may be high-risk if:
- You have a health problem, such as:
- Diabetes.
- Cancer.
- High blood pressure.
- Kidney disease.
- Epilepsy.
- You use alcohol or illegal drugs, or you smoke.
- You are younger than 17 or older than 35.
- You are pregnant with more than one baby (multiple pregnancy).
- You have had three or more miscarriages.
- Your baby has been found to have a genetic condition, such as Down syndrome, or a heart, lung, or kidney problem.
- You had a problem in a past pregnancy, such as:
- Preterm labor.
- Preeclampsia or seizures (eclampsia).
- Having a baby with a genetic problem, such as Down syndrome.
- You have an infection, such as HIV or hepatitis C. Other infections that can cause a problem include cytomegalovirus (CMV), chickenpox, rubella, toxoplasmosis, and syphilis.
- You are taking certain medicines, such as lithium, phenytoin (such as Dilantin), valproic acid (Depakene), or carbamazepine (such as Tegretol).
Other health problems can make your pregnancy high-risk.
These include heart valve problems,
sickle cell disease,
asthma,
lupus, and
rheumatoid arthritis. Talk to your doctor about any
health problems you have.
How will your doctor care for you during your pregnancy?
You will have more visits to the doctor than a woman who does not have a
high-risk pregnancy. You may have more
ultrasound tests to make sure that your baby is
growing well. You will have regular blood pressure checks. And your urine will
be tested to look for protein (a sign of preeclampsia) and urinary tract
infections.
How will your doctor care for you during your pregnancy? continued...
Tests for genetic or other problems also may be done,
especially if you are 35 or older or if you had a genetic problem in a past
pregnancy.
Your doctor will prescribe any medicine you may need,
such as for diabetes, asthma, or high blood pressure.
Talk to your
doctor about where he or she would like you to give birth. Your doctor may want
you to have your baby in a hospital that offers special care for women and
babies who may have problems.
If your doctor thinks that your
health or your baby's health is at risk, you may need to have the baby
early.
What type of doctor will you see for a high-risk pregnancy?
Some women will see a doctor who has extra training in
high-risk pregnancies. These doctors are called maternal-fetal specialists, or
perinatologists. You may see this doctor and your
regular doctor. Or the specialist may be your doctor throughout your pregnancy.
What can you do to help have a healthy pregnancy?
You can help yourself and your baby be as healthy as possible:
- Go to all your doctor visits so that you don't miss tests to catch any new problems.
- Eat a healthy diet that includes protein, milk and milk products, fruits, and vegetables. Talk to your doctor about any changes you may need in your diet.
- Take any medicines, iron, or vitamins that your doctor prescribes. Don't take any vitamins or medicines (including over-the-counter medicines) without talking to your doctor first.
- Take folic acid daily. Folic acid is a B vitamin. Taking folic acid before and during early pregnancy reduces your chance of having a baby with a neural tube defect or other birth defects.
- Follow your doctor's instructions for activity. Your doctor will let you know if you can work and exercise.
- Do not smoke. If you need help quitting, talk to your doctor about stop-smoking programs and medicines. Avoid other people's tobacco smoke.
- Do not drink alcohol.
- Stay away from people who have colds and other infections.
Your doctor may ask you to keep track of how much your
baby moves every day.
What symptoms should you watch for?
Like any
pregnant woman, you need to watch for any signs of problems. This doesn't mean
that you will have any problems. But if you have any of these symptoms, it's
important to get care quickly.
Call emergency services right away if you think you need emergency care. For example,
call if:
- You passed out (lost consciousness).
- You have severe vaginal bleeding.
- You have severe pain in your belly or pelvis.
- You have had fluid gushing or leaking from your vaginaand you know or think the umbilical cord is bulging into your vagina. If this happens, immediately get down on your knees so your rear end (buttocks) is higher than your head. This will decrease the pressure on the cord until help arrives.
Call your doctor now or seek
medical care right away if:
- You have signs of preeclampsia, such as:
- You have any vaginal bleeding.
- You have belly pain or cramping.
- You have a fever.
- You have had regular contractions (with or without pain) for an hour. This means that you have 8 or more in 1 hour or 4 or more in 20 minutes after you change your position and drink fluids.
- You have a sudden release of fluid from your vagina.
- You have low back pain or pelvic pressure that does not go away.
- You notice that your baby has stopped moving or is moving much less than normal.
7 Pregnancy Warning Signs
Some symptoms during pregnancy are par for the course, but others are cause for alarm. How do you know the difference?

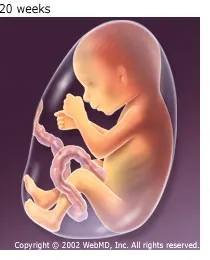
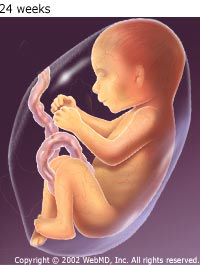
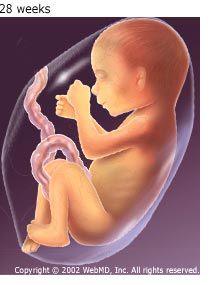
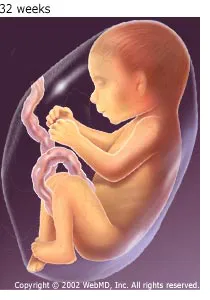
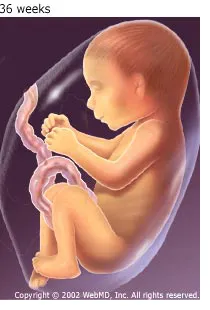
Stage 2 begins when the cervix is completely opened. At this point, your doctor will give you the OK to push. Your pushing, along with the force of your contractions, will propel your baby through the birth canal. The fontanels (soft spots) on your baby's head allow it to fit through the narrow canal.
A C-section may be planned or unplanned. In most cases, doctors do cesarean sections because of problems that arise during labor. Reasons you might need an unplanned C-section include:
You may wonder what symptoms during pregnancy warrant immediate medical attention and what symptoms can wait until your next prenatal visit.
Always ask your doctor at your visits about your concerns. But keep in mind some symptoms do need swift attention.
1. Bleeding
Bleeding means different things throughout your pregnancy. “If you are bleeding heavily and have severe abdominal pain and menstrual-like cramps or feel like you are going to faint during first trimester, it could be a sign of an ectopic pregnancy,” Peter Bernstein, MD, ob-gyn professor at New York's Albert Einstein College of Medicine and Montefiore Medical Center, says. Ectopic pregnancy, which occurs when the fertilized egg implants somewhere other than the uterus, can be life-threatening.
Heavy bleeding with cramping could also be a sign of miscarriagein first or early second trimester. By contrast, bleeding with abdominal pain in the third trimester may indicate placental abruption, which occurs when the placenta separates from the uterine lining.
“Bleeding is always serious,” women’s health expert Donnica Moore, MD, says. Any bleeding during pregnancy needs immediate attention. Call your doctor or go to the emergency room.
2. Severe Nausea and Vomiting
It's very common to have some nausea when you're pregnant. If it gets to be severe, that may be more serious.
“If
you can’t eat or drink anything, you run the risk of becoming
dehydrated,” Bernstein says. Being malnourished and dehydrated can harm
your baby.
If you experience severe nausea, tell your health care provider. Your doctor may prescribe medication or advise changing your diet.
3. Baby’s Activity Level Significantly Declines
What does it mean if your previously active baby seems to have less energy? It may be normal. But how can you tell?
Some
troubleshooting can help determine if there is a problem. Bernstein
suggests that you first drink something cold or eat something. Then lie
on your side to see if this gets the baby moving.
Counting
kicks can also help, Nicole Ruddock, MD, assistant professor of
maternal and fetal medicine at University of Texas Medical School at
Houston, says. “There is no optimal or critical number of movements,”
she says, “but generally you should establish a baseline and have a
subjective perception of whether your baby is moving more or less. As a
general rule, you should have 10 or more kicks in two hours. Anything
less should prompt a phone call to your doctor.”
Bernstein
says to call your doctor as soon as possible. Your doctor has
monitoring equipment that can be used to determine if the baby is moving
and growing appropriately.
4. Contractions Early in the Third Trimester
Contractions could be a sign of preterm labor. “But a lot of first-time moms may confuse true labor and false labor,” Ruddock says. False labor contractions
are called Braxton-Hicks contractions. They’re unpredictable,
non-rhythmic, and do not increase in intensity. “They will subside in an
hour or with hydration,” Ruddock says. “But regular contractions are about 10 minutes apart or less and increase in intensity.”
If you're in your third trimester
and think you're having contractions, call your doctor right away. If
it is too early for the baby to be born, your doctor may be able to stop
labor.
5. Your Water Breaks
You
walk into the kitchen for a drink and feel a flood of water rush down
your legs. “Your water could have broken,” Ruddock says, “but during
pregnancy the enlarged uterus can cause pressure on your bladder
too. So it could be urine leakage.” Ruddock says that sometimes water
breaking is a dramatic gush of fluid, but other times it is more subtle.
“If you are not sure if it is urine versus a true rupture of the membrane, go to the bathroom and empty your bladder," she says. "If the fluid continues, then you have broken your water.” Call your doctor or go to the hospital.
6. A Persistent Severe Headache, Abdominal Pain, Visual Disturbances, and Swelling During Your Third Trimester
These symptoms could be a sign of preeclampsia. That’s a serious condition that develops during pregnancy and is potentially fatal. The disorder is marked by high blood pressure and excess protein in your urine that typically occurs after the 20th week of pregnancy.
“Call your doctor right away and get your blood pressure tested,” Bernstein says. “Good prenatal care can help catch preeclampsia early.”
7. Flu Symptoms
Our experts say it’s important for pregnant women to get the flu vaccine since pregnant women are more likely to get sick and have serious complications from the flu than other women during flu season.
But if you do get the flu,
"don’t rush into a hospital or doctor’s office where you can spread it
to other pregnant women," Bernstein says. "Call your doctor first."
Does Bed Rest During Pregnancy Really Help?
If you've had problems during pregnancy, your doctor may have suggested bed rest. It may seem like a relief after the stress you've been under. Bed rest has been a way of treating pregnancy complications for more than a hundred years.
But
there's a problem. While bed rest is a common treatment, there's no
proof that it helps. It doesn't seem to protect your health or your
baby's. In fact, bed rest has risks itself. Doctors still prescribe it,
but more because of tradition than good evidence that it works.
Confused? Lots of women are. To help, here’s a rundown of what the research tells us about bed rest for pregnancy complications.
Why Is Bed Rest Prescribed?
Some doctors suggest bed rest for conditions like growth problems in the baby, high blood pressure or preeclampsia, vaginal bleeding from placenta previa or abruption, preterm labor, cervical insufficiency, threatened miscarriage,
and other problems. They hope that by taking it easy, you lower the
risk of preterm birth or pregnancy complications. Today, almost 1 out of
5 women is on restricted activity or bed rest at some point during her
pregnancy.
However, studies of bed rest have not
found evidence that bed rest helps with any of these conditions. It
doesn't lower the risk of complications or early delivery.
Many
doctors know that there's not good evidence that bed rest helps. But
they try it anyway because they think it's harmless. Unfortunately,
studies have found that bed rest poses real risks. They include:
- Blood clots
- Depression and anxiety
- Family stress
- Financial worries, especially if you have to stop working
- Low birth-weight for your baby
- Slower recovery after birth
- Weakened bones and muscles
The stricter a woman's bed rest, the worse these side effects seem to be, studies show.
At
this point, studies suggest that pregnant women -- even with
complications -- are better off continuing their normal routine than
resting. There's evidence that physical activity during pregnancy lowers the risk of problems like low birth-weight and preeclampsia.
What Should I Do if My Doctor Prescribes Bed Rest?
Feel
free to question your doctor's advice. Doctors should be willing to
explain their reasoning. It's important to get clear answers.
Things to ask your doctor include:
- Why are you recommending bed rest?
- How do you define bed rest? Lying in bed all day? Occasional breaks?
- Is bed rest really necessary? Are there other options?
- What are the specific benefits my baby and I will get from bed rest?
- Do those benefits outweigh the risks?
- What do the medical studies show?
- What are some potential problems from bed rest? For my baby? For me?
- Is there a maternal-fetal medicine specialist we could talk with?
If
you have concerns afterward, get a second opinion or talk to a
specialist. Your doctor should give you a clear reason for bed rest.
Tips for Getting Through Bed Rest
If
you and your doctor agree that you should give bed rest a try, ask more
questions. The term "bed rest" is vague. You need to know exactly what
your doctor expects. Ask questions like:
- How long will I need bed rest?
- Do I have to stay in bed all the time? Can I go to work?
- Can I get up to shower or use the bathroom?
- Can I do normal household chores and take care of my other kids?
- Should I avoid lifting anything heavy?
- Should I lie on one side or stay in a certain position?
- Is sexual activity OK? If so, what kinds and how much?
Bed
rest can be tough, physically and mentally. It's boring and stressful.
You need to focus on making it as bearable as you can. These tips may
help:
Schedule your day. Staying on schedule
will break up the day and fight boredom. Get dressed in the morning.
Keep a to-do list and plan activities for the day, such a reading,
watching a movie, or doing word games.
Do the exercises your doctor recommends. You need to keep up your muscle strength. Moving your legs will lower the risk of blood clots.
Have a support system. You need the help of family and friends to get through this. Have visitors. Keep in touch by phone, email, and text.
Eat well. Aim for a well-balanced diet with lots of fiber, and drink plenty of water. You'll lower the risk of constipation.
Let people help.
It may be hard to ask for help, but you must. If friends or family
members ask how they can help, offer specifics. Have them pick up
groceries or take your turn in carpool.
Learn something new. Start learning a new language, take a correspondence class, watch YouTube videos on how to draw or learn how to knit.
Morning Sickness
More than half of pregnant women have nausea and vomiting, especially during the first trimester. Despite its name, you can have morning sickness any time of day. It doesn't mean your baby is sick, and it doesn't hurt you or your baby. Pregnancynausea
is probably caused by the sudden increase of hormones in your body.
It's usually mild and goes away about midway through your pregnancy.
Some women never feel nauseous during their pregnancy.
Call Doctor If:
- You have flu-like symptoms, which may be a sign of illness.
- You feel dizzy or lethargic.
- You have severe vomiting constantly or several times a day.
- You can't keep down any fluids or foods and are losing weight.
- You think your nausea may be caused by iron in your prenatal vitamin.
- You want to take anti-nausea medication or try a treatment like acupuncture.
Step-by-Step Care:
- Eat five or six small meals instead of three big ones to avoid having an empty stomach.
- Take a multivitamin regularly. This may make morning sickness less severe. Don't take your vitamin on an empty stomach because it may worsen nausea.
- Avoid smells that upset your stomach.
- Eat saltine crackers, dry toast, or dry cereal before you get out of bed to calm your stomach.
- Avoid spicy and fatty foods.
- When you feel nauseous, eat bland foods that are easy to digest, like rice, bananas, chicken broth, gelatin, or Popsicles.
- Suck on ice or sip water, weak tea, or clear sodas when you feel nauseous.
What Is Hyperemesis Gravidarum?
Many pregnant women have morning sickness. But for a few, it’s much more intense. Less than 3% of pregnant women get something called hyperemesis gravidarum. There's no cure for it, but it's temporary, and there are ways to manage it.
What Is It?
When you have hyperemesis gravidarum, you vomit a lot, sometimes almost constantly. This can lead to problems like dehydration and weight loss. Morning sickness often fades by the end of the first trimester, but hyperemesis gravidarum usually lasts longer.
It generally strikes between the 4th and 6th week of pregnancy, and may be at its worst around weeks 9 to 13. The vomiting
is so severe, most women are unable to go about their typical daily
activities. Symptoms usually get better by the 20th week, but not
always.
Doctors don't know what causes it, but they believe it's related to a rise in hormone levels.
Women
who had the condition during their first pregnancy have a higher chance
of getting it again during the next one. There’s no known way to
prevent it, though taking a multivitamin before getting pregnant may help a little.
Complications
Hyperemesis gravidarum can cause problems for both you and your baby. It can affect:
- Your weight. Losing 5% is common.
- Your kidneys. They may stop working well, causing you to pee less than you should.
- Your mineral balance. You may have low levels of minerals, called electrolytes, that your body needs. They include sodium and potassium. When you don't have enough, it can cause dizziness, weakness, and changes in blood pressure.
- Your muscles. Malnutrition, electrolyte imbalance, and the need for bed rest can weaken your muscles.
- Your saliva. You may make too much. Swallowing it may make nausea even worse.
Your
doctor will need to help you manage this. Without treatment, there’s a
higher chance your baby will be born prematurely or have a low birth
weight. Either of these can put him at risk for health problems.
Treatments
Treatment
depends on your symptoms and how the condition is affecting your
health. Up to 5% of women with the condition need to check in to a
hospital. Your doctor may first recommend:
- Lifestyle changes. If you can eat, have smaller, more frequent meals. Drink smaller drinks, but drink more often, and through a straw. Try cold foods if hot ones trigger nausea. Your doctor may want you to drink electrolyte-replacement sports drinks and nutritional supplements. Get enough sleep and try to manage your stress.
- Ginger . Taking 1 to 1.5 grams a day in several small doses may help some women. You can get it in tea, lollipops, or supplements.
- Thiamine. This vitamin (also called vitamin B1) in doses of 1.5 milligrams a day may ease vomiting.
- Medications. Your doctor can prescribe one or more drugs to help you throw up less. You can take them by mouth, suppository, IV, or in a shot. Antacids can also help. Another possible treatment is IV steroids. Your doctor will make sure any medications you take are safe for your baby.
- If you're still throwing up and dehydrated, your doctor may recommend you check in to the hospital. Once there you may get:
- IV fluids. Doctors will give you saline and possibly electrolytes and vitamins to help keep you hydrated.
- Tube feeding. If you can’t keep anything down, the doctor may give you nutrition through a tube that goes through your nose and into your stomach. In extreme cases you may need a tube connected directly to your stomach or small intestine.
- IV feeding. This bypasses the stomach altogether.
Once you aren't vomiting so much and are able to hold down food and remain hydrated, you may be able to stop treatments.
Try to remember that it does eventually stop -- and the birth of your baby will follow.
Sex During and After Pregnancy
Pregnant women and their partners often wonder if it's safe to have sex during pregnancy. Will it result in miscarriage? Will it harm the unborn baby? Are there sex positions to avoid? Here's the information you've been looking for.
Is Sex Safe During Pregnancy?
Sex
is a natural, normal part of pregnancy -- if you're having a normal
pregnancy. Penetration and intercourse’s movement won't harm the baby, who is protected by your abdomen and the uterus’ muscular walls. Your baby is also cushioned by the amniotic sac’s fluid.
The contractions of orgasm aren't the same as labor contractions.
Still, as a general safety precaution, some doctors advise avoiding sex
in the final weeks of pregnancy, believing that hormones in semen
called prostaglandins can stimulate contractions. One exception may be for women who are overdue and want to induce labor.
Some doctors believe that prostaglandins in semen actually induce labor
in a full-term or past-due pregnancy, since the gel used to "ripen" the
cervix
and induce labor also contains prostaglandins. But other doctors
believe this semen/labor connection is only theoretical and that having
sex doesn't trigger labor.
As for orgasm, those contractions aren't the same as labor contractions. So there's no problem there.
When Not to Have Sex During Pregnancy
Your doctor may advise you not to have sex if you have any of the following types of high-risk pregnancy:
- You're at risk for miscarriage or history of past miscarriages
- You're at risk for preterm labor (contractions before 37 weeks of pregnancy)
- You're having vaginal bleeding, discharge, or cramping without a known cause
- Your amniotic sac is leaking fluid or has ruptured membranes
- Your cervix has opened too early in pregnancy
- Your placenta is too low in the uterus (placenta previa)
- You're expecting twins, triplets, or other "multiples"
Keep in mind, if your doctor says "no sex," that may include anything that involves orgasm or sexual arousal, not just intercourse.
Pregnancy Sex
Every woman's experiences during pregnancy are different -- including how she feels about sex.
For
some, desire fades during pregnancy. Other women feel more deeply
connected to their sexuality and more aroused when they're pregnant.
During
pregnancy, it's normal for sexual desire to come and go as your body
changes. You may feel self-conscious as your belly grows. Or you may
feel sexier with larger, fuller breasts.
Tell
your partner what you're feeling and what works. You may need to play
with positions, especially later in pregnancy, to find one that's both
comfortable and stimulating for you.
Avoid
lying flat on your back in the "missionary position" for sex after the
fourth month of pregnancy. That way, you can avoid the weight of the growing baby constricting major blood vessels.
Another
way to make sex more comfortable is to try lying sideways together. Or
you might try positioning yourself upright or sitting on top.
As always, if you're not absolutely sure about your partner's sexual history, use condoms. Pregnancy doesn't protect against sexually transmitted infections -- such as HIV, herpes, genital warts, or chlamydia -- and those infections can affect your baby.
Sex After Pregnancy
The
first six weeks after delivery are called the postpartum period. Sex
during this time may be the last thing on your mind. Reasons your desire
for sex may decrease are:
- Healing from an episiotomy (incision during vaginal delivery)
- Healing from abdominal incisions after cesarean birth
- Normal postpartum bleeding, common for four to six weeks after birth
- Fatigue after pregnancy and the birthing process
- Demands of your newborn (increased if you had twins or triplets)
- Changing hormone levels
- Sore breasts from breastfeeding
- Emotional issues, such as postpartum blues, anxiety over parenting, or relationship issues with the father
Intercourse is generally safe after any incisions have fully healed and you feel the delicate tissues of your vagina
have healed. This healing usually takes several weeks. You can ask your
doctor what she recommends. Most doctors will say wait at least 6 weeks
after delivery before intercourse. Equally important is feeling
emotionally ready, physically comfortable, and relaxed.
For both you and your partner, patience is a virtue. Given the realities and stresses of early parenthood, it can take up to a year for a couple's normal sex life to return in full bloom.
Common Pregnancy Pains and Their Causes
You will be visited with various kinds of discomforts during pregnancy
-- some fleeting, some more permanent. Some may occur in the early
weeks, while others emerge closer to the time of delivery. Others may
appear early and then go away, only to return later.
Every
woman's pregnancy is unique, so you may not experience all of the
changes described in this article. As always, if you notice any changes
that concern you, mention them to your health care provider. The pains listed below are considered a normal part of pregnancy.
Pregnancy Breast Changes
Most pregnant women will feel some changes in their breasts. Your breasts
will increase in size as your milk glands enlarge and the fat tissue
enlarges, causing breast firmness and tenderness typically during
pregnancy’s first and last few months. Bluish veins may also appear as
your blood
supply increases. Your nipples can also darken, and sometimes a thick
fluid called colostrum may leak from your breasts. All of these changes
are normal.
Recommendations:
- Wear a bra that provides firm support.
- Choose cotton bras or those made from natural fibers.
- Get a bigger bra as your breasts become larger and fuller. Your bra should fit well without irritating your nipples. Try maternity or nursing bras, which provide more support and can be used after pregnancy if you choose to breastfeed.
- Try wearing a bra during the night.
- Tuck a cotton handkerchief or gauze pad into each bra cup to absorb leaking fluid. You can also buy nursing pads in the drugstore or maternity/baby store that fit into your bra. Make sure to change these pads as needed so your skin doesn't get irritated.
- Wash your breasts with warm water and mild soap that will not cause dryness.
Pregnancy Fatigue
Feeling tired? That might be because your growing baby requires extra energy. Sometimes, it's a sign of anemia (low iron in the blood), which is common during pregnancy.
Recommendations:
- Get plenty of rest; go to bed earlier and take naps.
- Keep a regular schedule when possible.
- Pace yourself. Balance activity with rest.
- Moderate exercise daily boosts your energy level.
- Ask your health care provider to test your blood routinely for anemia.
Pregnancy Nausea or Vomiting
It's very common -- and normal -- to have an upset stomach when you're pregnant.
Chalk
it up to pregnancy's hormonal changes. It usually happens early in
pregnancy, while your body is adjusting to the higher hormone levels.
Good
news: Nausea usually disappears by the fourth month of pregnancy
(although in some cases it can persist throughout the pregnancy). It can
happen at any time of the day but may be worse in the morning, when
your stomach is empty (that why it's called "morning sickness") or if you aren't eating enough.
Recommendations:
- If nausea is a problem in the morning, eat dry foods like cereal, toast or crackers before getting out of bed. Try eating a high-protein snack such as lean meat or cheese before going to bed (protein takes longer to digest).
- If you are hungry but extremely nauseated, try the BRAT (bananas, rice and tea) diet as well as bland foods.
- Seabands offer some pregnant women comfort.
- Ginger may combat nausea.
- Eat small meals or snacks every two to three hours rather than three large meals. Eat slowly and chew your food completely.
- Sip on fluids throughout the day. Avoid large amounts of fluids at one time. Try cool, clear fruit juices, such as apple or grape juice.
- Avoid spicy, fried, or greasy foods.
- If you are bothered by strong smells, eat foods cold or at room temperature to minimize or avoid odors that bother you.
- Talk to your doctor about taking vitamin B6. Other natural treatments and prescription medications can provide relief.
- Contact your health care provider if your vomiting is constant or so severe that you can't keep fluids or foods down. This can cause dehydration and should be treated right away.
Pregnancy Frequent Urination
Your growing uterus and baby press against your bladder, causing a frequent need to urinate during the first trimester. This will happen again in the third trimester, when the baby's head drops into the pelvis before birth.
Recommendations:
- Don't wear tight-fitting underwear, pants, or pantyhose.
- If your urine burns or stings, it could be a sign of urinary tract infection. Contact your health care provider right away to treat it.
Pregnancy Headaches
Headaches can happen anytime during pregnancy. They can be caused by tension, congestion, constipation, or in some cases, preeclampsia (detected after 20 weeks).Recommendations:- Put an ice pack on your forehead or the back of your neck.
- Rest, sit, or lie quietly in a low-lit room. Close your eyes and try to relax your back, neck, and shoulders.
- Over-the-counter acetaminophen like Tylenol may help. But if your headaches don't go away, are severe, make you nauseous, or affect your vision, tell your doctor.
Pregnancy Bleeding and Swollen Gums
You may not have expected pregnancy to affect your mouth.
But your blood circulation and hormone levels can make your gums tender
and swollen, and you may notice they bleed more easily. You may also
develop nose bleeds.
Recommendations:
- Get a dental checkup early in your pregnancy to make sure your teeth and mouth are healthy. See your dentist if you notice a particular problem.
- Brush your teeth and floss regularly.
Pregnancy Constipation
Constipated? It can happen during pregnancy for a couple of reasons.
Your hormones, as well as vitamins and iron supplements, may cause constipation
(difficulty passing stool or incomplete or infrequent passage of hard
stools). Pressure on your rectum from your uterus may also cause
constipation.
Recommendations:
- Add more fiber (such as whole grain foods, fresh fruits, and vegetables) to your diet.
- Drink plenty of fluids daily (at least 6-8 glasses of water and 1-2 glasses of fruit or prune juice).
- Drink warm liquids, especially in the morning.
- Exercise daily.
- Avoid straining when you have a bowel movement.
- Discuss the use of a laxative or stool softener with your health care provider.
Pregnancy Dizziness (Feeling Faint)
Dizziness can occur anytime during middle to late pregnancy. Here's why it happens:
- The hormone progesterone dilates blood vessels so blood tends to pool in the legs.
- More blood is also going to your growing uterus. This can cause a drop in blood pressure, especially when changing positions -- and that can make you dizzy. If your blood sugar levels get too low, you may feel faint.
Recommendations:
- Move around often when standing for long periods of time.
- Lie on your left side to rest. This helps circulation throughout your body.
- Avoid sudden movements. Move slowly when standing from a sitting position.
- Eat regular, small meals throughout the day to prevent low blood sugar.
- Drink plenty of water.
Difficulty Sleeping During Pregnancy
Finding a comfortable resting position can become difficult later in pregnancy.
Recommendations:
- Don't take sleep medication.
- Try drinking warm milk at bedtime.
- Try taking a warm shower or bath before bedtime.
- Use extra pillows for support while sleeping. Lying on your side, place a pillow under your head, abdomen, behind your back and between your knees to prevent muscle strain and help you get the rest you need.
- You will probably feel better lying on your left side; this improves circulation of blood throughout your body.
Pregnancy Heartburn or Indigestion
Heartburn
is a burning feeling that starts in the stomach and seems to rise up to
the throat. During pregnancy, changing hormone levels slow down your digestive system, weaken the stomach sphincter, and your uterus can crowd your stomach, pushing stomach acids upward.
Recommendations:
- Eat several small meals each day instead of three large meals.
- Eat slowly.
- Drink warm liquids.
- Avoid fried, spicy, or rich foods, or any foods that seem to give you indigestion.
- Don't lie down right after eating.
- Keep the head of your bed higher than the foot of your bed. Or, place pillows under your shoulders to prevent stomach acids from rising into your throat.
- Don't mix fatty foods with sweets in one meal, and try to separate liquids and solids at meals.
- Try heartburn relievers such as Tums, Maalox, Titralac, Mylanta, Riopan, or Gaviscon.
Pregnancy Hemorrhoids
Hemorrhoids are swollen veins that appear as painful lumps on the anus. During pregnancy, they may form as a result of increased circulation and pressure on the rectum and vagina from your growing baby.
Recommendations:
- Try to avoid constipation. Constipation can cause hemorrhoids and will make them more painful.
- Avoid sitting or standing for long periods of time; change your position frequently.
- Don't strain during a bowel movement.
- Apply ice packs or cold compresses to the area or take a warm bath a few times a day to provide relief.
- Avoid tight-fitting underwear, pants, or pantyhose.
- If you still need more help, consult your health care provider.
Pregnancy Varicose Veins
Pregnancy may affect your circulation, which can enlarge or swell your legs' veins.
Recommendations:
Although varicose veins are usually hereditary, here are some preventive tips:
- Avoid standing or sitting in one place for long periods. It's important to get up and move around often.
- Avoid remaining in any position that might restrict the circulation in your legs (such as crossing your legs while sitting).
- Elevate your legs and feet while sitting.
- Exercise regularly.
- Wear support hose but avoid any leg wear that is too tight or constraining.
Pregnancy Leg Cramps
Pressure from your growing uterus can cause leg cramps or sharp pains down your legs.
Recommendations:
- Be sure to eat and drink foods that are rich in calcium (such as milk, broccoli or cheese).
- Wear comfortable, low-heeled shoes.
- Try wearing support hose, but avoid any leg wear that is too tight.
- Elevate your legs when possible; avoid crossing your legs.
- Exercise daily.
- Stretch your legs before going to bed.
- Avoid lying on your back, since the weight of your body and the pressure of your enlarged uterus can slow the circulation in your legs, causing cramps.
- Gently stretch any muscle that becomes cramped by straightening your leg, flexing your foot, and pulling your toes toward you.
- Massage the cramp or apply heat or a hot water bottle to the sore area.
Pregnancy Nasal Congestion
You
may have a stuffy nose or feel like you have a cold. Pregnancy hormones
sometimes dry out the nose's lining, making it inflamed and swollen.
Recommendations:
- Apply a warm, wet washcloth to your cheeks, eyes, and nose to reduce congestion.
- Avoid using nasal sprays unless prescribed by your doctor because they can aggravate your symptoms.
- Drink plenty of fluids (at least 6-8 glasses of fluids a day) to thin mucus.
- Elevate your head with an extra pillow while sleeping to prevent mucus from blocking your throat.
- Use a humidifier or vaporizer to add moisture to the air.
- Take a warm shower or bath.
Shortness of Breath During Pregnancy
Shortness of breath can happen due to increased upward pressure from the uterus and changes in physiologic lung function.
Recommendations:
- When walking, slow down and rest a few moments.
- Raise your arms over your head (this lifts your rib cage and allows you to breathe in more air).
- Avoid lying flat on your back, and try sleeping with your head elevated.
- If prolonged shortness of breathing continues or you experience sharp pain when inhaling, contact your health care provider. You could have a pulmonary embolism (blood clot in the lungs).
Pregnancy Stretch Marks
Stretch marks are a type of scar tissue that forms when the skin's normal elasticity is not enough for the stretching that occurs during pregnancy. They usually appear on the abdomen and can also appear on the breasts, buttocks or thighs.Though they won't disappear completely, stretch marks will fade after delivery. Stretch marks affect the surface under the skin and are not preventable.Recommendations:- Be sure that your diet contains enough sources of the nutrients needed for healthy skin (especially vitamins C and E).
- Apply lotion to your skin to keep it soft and reduce dryness.
- Exercise daily.
Swelling in the Feet and Legs During Pregnancy
Pressure
from your growing uterus on the blood vessels carrying blood from the
lower body causes fluid retention. The result is swelling (edema) in the legs and feet.
Recommendations:
- Try not to stay on your feet for long periods of time. Avoid standing in one place.
- Drink plenty of fluids (at least 6-8 glasses of fluids a day).
- Avoid foods high in salt (sodium).
- Elevate your legs and feet while sitting. Avoid crossing your legs.
- Wear loose, comfortable clothing; tight clothing can slow circulation and increase fluid retention.
- Don't wear tight shoes; choose supportive shoes with low, wide heels.
- Keep your diet rich in protein; too little protein can cause fluid retention.
- Notify your health care provider if your hands or face swell. This may be a warning sign of preeclampsia.
- Rest on your side during the day to help increase blood flow to your kidneys.
Vaginal Discharge During Pregnancy
Normal vaginal secretions increase during pregnancy due to greater blood supply and hormones. Normal vaginal discharge is white or clear, isn't irritating, is odorless, and may look yellow when dry on your underwear or panty liners.
Recommendations:
- Choose cotton underwear or brands made from natural fibers.
- Avoid tight-fitting jeans or pants.
- Do not douche. Douching can introduce air into your circulatory system or break your bag of waters in later pregnancy.
- Clean the vaginal area often with soap and water.
- Wipe yourself from front to back.
- Contact your health care provider if you have burning, itching, irritation or swelling, bad odor, bloody discharge, or bright yellow or green discharge (these symptoms could be a sign of infection).
Pregnancy Backaches
Backaches are usually caused by the strain put on the back muscles, changing hormone levels, and changes in your posture.Recommendations:- Wear low-heeled (but not flat) shoes.
- Avoid lifting heavy objects.
- Squat down with your knees bent when picking things up instead of bending down at the waist.
- Don't stand on your feet for long periods. If you need to stand for long periods, place one foot on a stool or box for support.
- Sit in a chair with good back support, or place a small pillow behind your lower back. Also, place your feet on a footrest or stool.
- Check that your bed is firm. If needed, put a board between the mattress and box spring.
- Sleep on your left or right side with a pillow between your legs for support.
- Apply a hot water bottle or heating pad on low setting to your back, take a warm bath or shower, or try massage.
- Perform exercises, as advised by your health care provider, to make your back muscles stronger and help relieve the soreness.
- Maintain good posture. Standing up straight will ease the strain on your back.
- Contact your health care provider if you have a low backache that goes around your stomach and does not go away within one hour after you change position or rest. This might be a sign of premature labor.
Abdominal Pain or Discomfort
Sharp, shooting pains on either side of your stomach may result from the stretching tissue supporting your growing uterus. These pains may also travel down your thigh and into your leg.
Recommendations:
- Change your position or activity until you are comfortable; avoid sharp turns or movements.
- If you have a sudden pain in your abdomen, bend forward to the point of pain to relieve tension and relax the tissue.
- Apply a hot water bottle or heating pad to your back, or take a warm bath or shower.
- Try a massage.
- Make sure you are getting enough fluids.
- Take Tylenol (acetaminophen) occasionally.
- Contact your health care provider if the pain is severe or constant or if you are less than 36 weeks pregnant and you have signs of labor. (Signs of labor include repetitive cramping like contractions.)
Braxton-Hicks Contractions
The uterine muscles will contract (tighten) starting as early as the second trimester of pregnancy on. Irregular, infrequent contractions are called Braxton-Hickscontractions (also known as "false labor pains"). These are normal during pregnancy.
Recommendations:
- Try to relax
- Change positions. Sometimes this can ease the contractions.
- Call your doctor if they do not go away.
Bleeding During Pregnancy
Bleeding during pregnancy is common, especially during the first trimester,
and usually it's no cause for alarm. But because bleeding can sometimes
be a sign of something serious, it's important to know the possible
causes, and get checked out by your doctor to make sure you and your
baby are healthy.
Bleeding in the First Trimester
About 20% of women have some bleeding during the first 12 weeks of pregnancy. Possible causes of first trimester bleeding include:
Implantation bleeding.
You may experience some normal spotting within the first six to 12 days
after you conceive as the fertilized egg implants itself in the lining
of the uterus. Some women don't realize they are pregnant because they
mistake this bleeding for a light period. Usually the bleeding is very
light and lasts from a few hours to a few days.
Miscarriage.
Because miscarriage is most common during the first 12 weeks of
pregnancy, it tends to be one of the biggest concerns with first
trimester bleeding. About half of women who bleed in pregnancy
eventually miscarry, but that doesn't necessarily mean that if you're
bleeding you've lost the baby, especially if you don't have any other
symptoms.
Other symptoms of miscarriage are strong cramps in the lower abdomen and tissue passing through the vagina.
Ectopic pregnancy.
In an ectopic pregnancy, the fertilized embryo implants outside of the
uterus, usually in the fallopian tube. If the embryo keeps growing, it
can cause the fallopian tube to burst, which can be life-threatening to
the mother. Although ectopic pregnancy is potentially dangerous, it only
occurs in about 2% of pregnancies.
Other symptoms of ectopic pregnancy are strong cramps or pain in the lower abdomen, and lightheadedness.
Molar pregnancy
(also called gestational trophoblastic disease). This is a very rare
condition in which abnormal tissue grows inside the uterus instead of a
baby. In rare cases, the tissue is cancerous and can spread to other
parts of the body.
Other symptoms of molar pregnancy are severe nausea and vomiting, and rapid enlargement of the uterus.
Additional causes of bleeding in early pregnancy include:
- Cervical changes. During pregnancy, extra blood flows to the cervix. Intercourse or a Pap test, which cause contact with the cervix, can trigger bleeding. This type of bleeding isn't cause for concern.
- Infection. Any infection of the cervix, vagina, or a sexually transmitted infection (such as chlamydia, gonorrhea, or herpes) can cause bleeding in the first trimester.
Bleeding in the Second and Third Trimesters
Abnormal
bleeding in late pregnancy may be more serious, because it can signal a
problem with the mother or baby. Call your doctor as soon as possible
if you experience any bleeding in your second or third trimester.
Possible causes of bleeding in late pregnancy include:
Placenta previa.
This condition occurs when the placenta sits low in the uterus and
partially or completely covers the opening of the birth canal. Placenta
previa is very rare in the late third trimester, occurring in only one
in 200 pregnancies. A bleeding placenta previa, which can be painless,
is an emergency requiring immediate medical attention.
Placental abruption. In about 1% of pregnancies, the placenta detaches from the wall of the uterus before or during labor and blood pools between the placenta and uterus. Placental abruption can be very dangerous to both the mother and baby.
Other signs and symptoms of placental abruption are abdominal pain, clots from the vagina, tender uterus, and back pain.
Uterine rupture.
In rare cases, a scar from a previous C-section can tear open during
pregnancy. Uterine rupture can be life-threatening, and requires an
emergency C-section.
Other symptoms of uterine rupture are pain and tenderness in the abdomen.
Vasa previa.
In this very rare condition, the developing baby's blood vessels in the
umbilical cord or placenta cross the opening to the birth canal. Vasa
previa can be very dangerous to the baby because the blood vessels can
tear open, causing the baby to bleed severely and lose oxygen.
Other signs of vasa previa include abnormal fetal heart rate and excessive bleeding.
Premature labor.Vaginal bleeding
late in pregnancy may just be a sign that your body is getting ready to
deliver. A few days or weeks before labor begins, the mucus plug that
covers the opening of the uterus will pass out of the vagina, and it
will usually have small amounts of blood in it (this is known as "bloody
show"). If bleeding and symptoms of labor begin before the 37th week of
pregnancy, contact your doctor right away because you might be in
preterm labor.
Other symptoms of preterm labor include contractions, vaginal discharge, abdominal pressure, and ache in the lower back.
Additional causes of bleeding in late pregnancy are:
- Injury to the cervix or vagina
- Polyps
- Cancer
What to Do If You Have Abnormal Bleeding During Pregnancy
Because
vaginal bleeding in any trimester can be a sign of a problem, call your
doctor. Wear a pad so that you can keep track of how much you're
bleeding, and record the type of blood (for example, pink, brown, or
red; smooth or full of clots). Bring any tissue that passes through the
vagina to your doctor for testing. Don't use a tampon or have sex while you are still bleeding.
You should expect to receive an ultrasound
to identify what the underlying cause of your bleeding may be. Vaginal
and abdominal ultrasounds are often performed together as part of a full
evaluation.
Go to the emergency room or call 911
right away if you are experiencing any of the following symptoms, which
could be signs of a miscarriage or other serious problem:
- Severe pain or intense cramps low in the abdomen
- Severe bleeding, whether or not there is pain
- Discharge from the vagina that contains tissue
- Dizziness or fainting
- A fever of more than 100.4 or more degrees Fahrenheit and/or chills.
Anemia in Pregnancy
When you're pregnant, you may develop anemia. When you have anemia, your blood doesn't have enough healthy red blood cells to carry oxygen to your tissues and to your baby.
During pregnancy, your body produces more blood to support the growth of your baby. If you're not getting enough iron or certain other nutrients, your body might not be able to produce the amount of red blood cells it needs to make this additional blood.
It's
normal to have mild anemia when you are pregnant. But you may have more
severe anemia from low iron or vitamin levels or from other reasons.
Anemia
can leave you feeling tired and weak. If it is severe but goes
untreated, it can increase your risk of serious complications like
preterm delivery.
Here's what you need to know about the causes, symptoms, and treatment of anemia during pregnancy.
Types of Anemia During Pregnancy
Several types of anemia can develop during pregnancy. These include:
- Iron-deficiency anemia
- Folate-deficiency anemia
- Vitamin B12 deficiency
Here's why these types of anemia may develop:
Iron-deficiency anemia. This type of anemia occurs when the body doesn't have enough iron to produce adequate amounts of hemoglobin. That's a protein in red blood cells. It carries oxygen from the lungs to the rest of the body.
In iron-deficiency anemia, the blood cannot carry enough oxygen to tissues throughout the body.
Iron deficiency is the most common cause of anemia in pregnancy.
Folate-deficiency anemia. Folate, also called folic acid, is a type of B vitamin. The body needs folate to produce new cells, including healthy red blood cells.
During
pregnancy, women need extra folate. But sometimes they don't get enough
from their diet. When that happens, the body can't make enough normal
red blood cells to transport oxygen to tissues throughout the body.
Folate deficiency can directly contribute to certain types of birth defects, such as neural tube abnormalities (spina bifida) and low birth weight.
Vitamin B12 deficiency. The body needs vitamin B12
to form healthy red blood cells. When a pregnant woman doesn't get
enough vitamin B12 from her diet, her body can't produce enough healthy
red blood cells. Women who don't eat meat, poultry, dairy products, and
eggs have a greater risk of developing vitamin B12 deficiency, which may
contribute to birth defects, such as neural tube abnormalities, and
could lead to preterm labor.
Blood loss during and after delivery can also cause anemia.
Risk Factors for Anemia in Pregnancy
All
pregnant women are at risk for becoming anemic. That's because they
need more iron and folic acid than usual. But the risk is higher if you:
- Are pregnant with multiples (more than one child)
- Have had two pregnancies close together
- Vomit a lot because of morning sickness
- Are a pregnant teenager
- Don't eat enough foods that are rich in iron
- Had anemia before you became pregnant
Symptoms of Anemia During Pregnancy
The most common symptoms of anemia during pregnancy are:
- Pale skin, lips, and nails
- Feeling tired or weak
- Dizziness
- Shortness of breath
- Rapid heartbeat
- Trouble concentrating
In
the early stages of anemia, you may not have obvious symptoms. And many
of the symptoms are ones that you might have while pregnant even if
you're not anemic. So be sure to get routine blood tests to check for
anemia at your prenatal appointments.
Risks of Anemia in Pregnancy
Severe or untreated iron-deficiency anemia during pregnancy can increase your risk of having:
- A preterm or low-birth-weight baby
- A blood transfusion (if you lose a significant amount of blood during delivery)
- Postpartum depression
- A baby with anemia
- A child with developmental delays
Untreated folate deficiency can increase your risk of having a:
- Preterm or low-birth-weight baby
- Baby with a serious birth defect of the spine or brain (neural tube defects)
Untreated vitamin B12 deficiency can also raise your risk of having a baby with neural tube defects.
Tests for Anemia
During
your first prenatal appointment, you'll get a blood test so your doctor
can check whether you have anemia. Blood tests typically include:
- Hemoglobin test. It measures the amount of hemoglobin -- an iron-rich protein in red blood cells that carries oxygen from the lungs to tissues in the body.
- Hematocrit test. It measures the percentage of red blood cells in a sample of blood.
If
you have lower than normal levels of hemoglobin or hematocrit, you may
have iron-deficiency anemia. Your doctor may check other blood tests to
determine if you have iron deficiency or another cause for your anemia.
Even
if you don't have anemia at the beginning of your pregnancy, your
doctor will most likely recommend that you get another blood test to
check for anemia in your second or third trimester.
Treatment for Anemia
If you
are anemic during your pregnancy, you may need to start taking an iron
supplement and/or folic acid supplement in addition to your prenatal vitamins. Your doctor may also suggest that you add more foods that are high in iron and folic acid to your diet.
In
addition, you'll be asked to return for another blood test after a
specific period of time so your doctor can check that your hemoglobin
and hematocrit levels are improving.
To treat vitamin B12 deficiency, your doctor may recommend that you take a vitamin B12 supplement.
The doctor may also recommend that you include more animal foods in your diet, such as:
- meat
- eggs
- dairy products
Your OB may refer you to a hematologist, a doctor who specializes in
anemia/ blood issues. These specialist may see you throughout the
pregnancy and help your OB manage the anemia.
Preventing Anemia
To
prevent anemia during pregnancy, make sure you get enough iron. Eat
well-balanced meals and add more foods that are high in iron to your
diet.
Aim for at least three servings a day of iron-rich foods, such as:
- lean red meat, poultry, and fish
- leafy, dark green vegetables (such as spinach, broccoli, and kale)
- iron-enriched cereals and grains
- beans, lentils, and tofu
- nuts and seeds
- eggs
Foods that are high in vitamin C can help your body absorb more iron. These include:
- citrus fruits and juices
- strawberries
- kiwis
- tomatoes
- bell peppers
Try
eating those foods at the same time that you eat iron-rich foods. For
example, you could drink a glass of orange juice and eat an
iron-fortified cereal for breakfast.
Also, choose foods that are high in folic acid to help prevent folate deficiency. These include:
- leafy green vegetables
- citrus fruits and juices
- fortified breads and cereals
- dried beans
Follow your doctor's instructions for taking a prenatal vitamin that contains a sufficient amount of iron and folic acid.
Vegetarians
and vegans should talk with their doctor about whether they should take
a vitamin B12 supplement when they're pregnant and breastfeeding.
What to Know About Ectopic Pregnancy
In a normal pregnancy, your ovary releases an egg into your fallopian tube. If the egg meets with a sperm, the fertilized egg moves into your uterus to attach to its lining and continues to grow for the next 9 months.
But in up to 1 of every 50 pregnancies, the fertilized egg stays in your fallopian tube. In that case, it's called an ectopic pregnancy or a tubal pregnancy. In rare cases, the fertilized egg attaches to one of your ovaries, another organ in your abdomen, the cornua (or horn) of the uterus or even the cervix.
In any case, instead of celebrating your pregnancy, you find your life
is in danger. Ectopic pregnancies require emergency treatment.
Most
often, ectopic pregnancy happens within the first few weeks of
pregnancy. You might not even know you're pregnant yet, so it can be a
big shock. Doctors usually discover it by the 8th week of pregnancy.
Ectopic
pregnancies can be scary and sad. The baby probably can't survive --
though in extremely rare cases he or she might. (This is not possible in
a tubal pregnancy, cornual or cervical ) So it's a loss that may take
some time to get over. It may comfort you to know that if you have an
ectopic pregnancy, you'll likely be able to have a healthy pregnancy in
the future.

Symptoms of an Ectopic Pregnancy
- Light vaginal bleeding
- Nausea and vomiting with pain
- Lower abdominal pain
- Sharp abdominal cramps
- Pain on one side of your body
- Dizziness or weakness
- Pain in your shoulder, neck, or rectum
- If the fallopian tube ruptures, the pain and bleeding could be severe enough to cause fainting.
If you are experiencing the symptoms listed above, contact your health care
provider immediately and go to the emergency room. Getting to the
hospital quickly is important to reduce the risk of hemorrhaging (severe
bleeding) and to preserve your fertility.
Causes of an Ectopic Pregnancy
One
cause of an ectopic pregnancy is a damaged fallopian tube that doesn't
let a fertilized egg into your uterus, so it implants in the fallopian
tube or somewhere else.
You might not ever know what caused an ectopic pregnancy. But you are higher risk if you have:
- Current use of an intrauterine device (IUD), a form of birth control.
- History of pelvic inflammatory disease (PID)
- Sexually-transmitted diseases such as chlamydia and gonorrhea
- Congenital abnormality (problem present at birth) of the fallopian tube
- History of pelvic surgery (because scarring may block the fertilized egg from leaving the fallopian tube)
- History of ectopic pregnancy
- Unsuccessful tubal ligation (surgical sterilization) or tubal ligation reversal
- Use of fertility drugs
- Infertility treatments such as in vitro fertilization (IVF)
Diagnosing an Ectopic Pregnancy
Once you arrive at the hospital, a pregnancy test, a pelvic exam, and an ultrasound test may be performed to view the uterus’ condition and fallopian tubes.
If an ectopic pregnancy has been confirmed, the health care provider will decide on the best treatment based on your medical condition and your future plans for pregnancy.
Treating an Ectopic Pregnancy
If
the doctor suspects that the fallopian tube has ruptured, emergency
surgery is necessary to stop the bleeding. In some cases, the fallopian
tube and ovary may be damaged and will have to be removed.
If
the fallopian tube has not ruptured and the pregnancy has not
progressed very far, laparoscopic surgery may be all that is needed to
remove the embryo and repair the damage. A laparoscope is a thin,
flexible instrument inserted through small incisions in the abdomen.
During this surgery, a tiny incision is made in the fallopian tube and
the embryo is removed, preserving the fallopian tube’s integrity.
In some cases, medication
may be used to stop the growth of pregnancy tissue. This treatment
option may be appropriate if the tube is not ruptured and the pregnancy
has not progressed very far.
After medical treatment for an ectopic pregnancy, you will usually have to have additional blood tests to make sure that the entire tubal pregnancy was removed. The blood tests detect the hCG level, the hormone that is produced during pregnancy.
Getting Pregnant After an Ectopic Pregnancy
Most
women who have an ectopic pregnancy have normal pregnancies and births
in the future, even if a fallopian tube was removed. As long as you have
one normally working fallopian tube, you can get pregnant. If the ectopic pregnancy was caused by a treatable illness, such as a sexually transmitted disease,
getting treated for it can improve your chances of a successful
pregnancy. The infection is not what caused the ectopic – it is the
scarring that occurs due to the infection. Treatment of the infection
does not get rid of the damage already done.
Talk
with your doctor about how long to wait after an ectopic pregnancy
before trying to conceive again. Some doctors suggest waiting 3 to 6
months.
After an ectopic pregnancy, take the time you
need to heal your body and mind. Above all, don't blame yourself.
Counseling or pregnancy loss support groups can help you and your
partner cope. Ask your doctor about groups near you.
SECOND TRIMESTER(3-6 MONTHS)OF PREGNANCY:
Second Trimester of Pregnancy
As you enter your second trimester of pregnancy, the morning sickness and fatigue
that plagued you during the last three months should be fading, leaving
you feeling more energetic and like your old self again.
The second trimester is, for many women, the easiest three months of pregnancy. Take the time now, while you're feeling better and your energy is up, to start planning for your baby's arrival.
During the second trimester, your baby is growing quickly. Between your 18th and 22nd week of pregnancy you'll have an ultrasound so your doctor can see how your baby is progressing. You also can learn the sex of your baby, unless you'd rather be surprised.
Although you should be feeling better now, big changes are still taking place inside your body. Here's what you can expect.
Changes in Your Body
Backache. The extra weight
you've gained in the last few months is starting to put pressure on
your back, making it achy and sore. To ease the pressure, sit up
straight and use a chair that provides good back support. Sleep
on your side with a pillow tucked between your legs. Avoid picking up
or carrying anything heavy. Wear low-heeled, comfortable shoes with good
arch support. If the pain is really uncomfortable, ask your partner to
rub the sore spots, or treat yourself to a pregnancy massage.
Bleeding gums. About half of pregnant women develop swollen, tender gums. Hormone changes are sending more blood
to your gums, making them more sensitive and causing them to bleed more
easily. Your gums should go back to normal after your baby is born. In
the meantime, use a softer toothbrush and be gentle when you floss, but don't skimp on dental hygiene. Studies show that pregnant women with gum disease (periodontal disease) may be more likely to go into premature labor and deliver a low-birth-weight baby.
Breast enlargement. Much of the breast tenderness you experienced during the first trimester should be wearing off, but your breasts
are still growing as they prepare to feed your baby. Going up a bra
size (or more) and wearing a good support bra can make you feel more
comfortable.
Congestion and nosebleeds.
Hormonal changes cause the mucus membranes lining your nose to swell,
which can lead to a stuffy nose and make you snore at night. These
changes may also make your nose bleed more easily. Before using a decongestant,
check with your doctor. Saline drops and other natural methods may be
safer ways to clear congestion during pregnancy. You can also try using a
humidifier to keep the air moist. To stop a nosebleed, keep your head
up straight (don't tilt it back) and apply pressure to the nostril for a
few minutes until the bleeding stops.
Discharge. It's normal to see a thin, milky white vaginal discharge
(called leukorrhea) early in your pregnancy. You can wear a panty liner
if it makes you feel more comfortable, but don't use a tampon because
it can introduce germs into the vagina. If the discharge is foul-smelling, green or yellow, bloody, or if there's a lot of clear discharge, call your doctor.
Frequent urination. Your uterus will rise away from the pelvic cavity during the second trimester, giving you a brief break from having to keep going to the bathroom. Don't get too comfortable, though. The urge to go will come back during the last trimester of your pregnancy.
Hair growth. Pregnancy hormones can boost hair
growth -- and not always where you want it. The hair on your head will
become thicker. You may also be seeing hair in places you never had it
before, including your face, arms, and back. Shaving and tweezing might
not be the easiest options, but they're probably your safest bets right
now. Many experts don't recommend laser hair removal, electrolysis, waxing, or depilatories during pregnancy, because research still hasn't proven that they are safe for the baby. Check to see what your doctor recommends.
Headache.Headaches
are one of the most common pregnancy complaints. Try to get plenty of
rest, and practice relaxation techniques, such as deep breathing. Aspirin and ibuprofen shouldn’t be taken during pregnancy, but your doctor may say it's OK for you to take acetaminophen if you're really uncomfortable.
Heartburn and constipation. These are caused by your body making more of a hormone called progesterone. This hormone relaxes certain muscles, including the ring of muscle in your lower esophagus that normally keeps food and acids down in your stomach, and the ones that move digested food through your intestines. To relieve heartburn,
try eating more frequent, smaller meals throughout the day and avoid
greasy, spicy, and acidic foods (such as citrus fruits). For constipation, get more fiber and drink extra fluids to keep things moving more smoothly. Physical activity will also help move things along.
Hemorrhoids.Hemorrhoids are actually varicose veins -- swollen blue or purple veins that form around the anus. These veins may enlarge during pregnancy, because extra blood is flowing through them and there is increased pressure on them from the growing uterus. Varicose veins can be itchy and uncomfortable. To relieve them, try sitting in a warm tub or sitz bath. Ask your doctor whether you can use an over-the-counter hemorrhoid ointment.
Quickening.
By the midpoint of your pregnancy (20 weeks) you will probably have
started to feel the first delicate flutters of movement in your abdomen,
which is often called "quickening." If you aren't feeling your baby
move yet, don't worry. Some women don't experience quickening until
their sixth month of pregnancy.
Skin changes.
Pregnant women often look as though they are "glowing" because changing
hormone levels make the skin on the face appear flushed. An increase in
the pigment melanin can also lead to brown marks on the face (often
called the "mask of pregnancy") and a dark line (linea nigra) down the
middle of the abdomen. All of these skin changes should fade after the
baby is born. In the meantime, you can use makeup
to conceal them. Your skin is also more sensitive to the sun right now,
so make sure to wear a broad-spectrum (UVA/UVB protection) sunscreen
with an SPF of at least 30 whenever you go outside. Limit your time in
the sun, especially between 10 a.m. and 2 p.m., wearing long-sleeved
clothes, pants, a broad-brimmed hat, and sunglasses. You may also notice thin, reddish-purple lines on your abdomen, breasts, or thighs. These stretch marks
emerge as your skin expands to accommodate your growing belly. Although
many creams and lotions claim to prevent or eliminate stretch marks,
there is little evidence that they actually do. Using a moisturizer can
help soften your skin and reduce itchiness. Most stretch marks should
fade on their own after you deliver.
Spider and varicose veins. Your circulation has
increased to send extra blood to your growing baby. That excess blood
flow can cause tiny red veins, known as spider veins, to appear on your
skin. These veins should eventually fade once your baby is born.
Pressure on your legs from your growing baby can also slow blood flow to
your lower body, causing the veins in your legs to become swollen and
blue or purple. These are called varicose veins. Although there's no way
to avoid varicose veins, you can prevent them from getting worse by
getting up and moving throughout the day and propping up your legs on a
stool whenever you have to sit for long periods of time. Wear support
hose for extra support. Varicose veins should improve within three
months after you deliver.
Weight gain.Morning sickness usually diminishes by the end of the first trimester. After that, your appetite should return, and will probably grow. Although food
is looking much more appetizing, be aware of how much you're eating.
You only need about an extra 300 to 500 calories a day during the second
trimester, and you should be gaining about 1/2 to 1 pound a week.
Red Flag Symptoms
Any
of these symptoms could be a sign that something is wrong with your
pregnancy. Don't wait for your prenatal visit to talk about it. Call
your doctor right away if you experience:
- Severe abdominal pain or cramping
- Bleeding
- Severe dizziness
- Rapid weight gain (more than 6.5 pounds per month) or too little weight gain (less than 10 pounds at 20 weeks into the pregnancy)
Your Pregnancy Week by Week: Weeks 13-16
FOURTH MONTH:
Week 13
Baby: Your baby is growing quickly! Eyes are moving into position, the ankles and wrists have formed, and though the head is still disproportionately big, the rest of the body is starting to catch up.
Mom-to-be: Your uterus has grown a lot. It's filling your pelvis now and starting to grow upward into your abdomen. It probably feels like a soft, smooth ball. If you haven't gained any weight yet because of morning sickness, you'll begin to now as you start to feel better.
Tip for the Week: Suggest that your partner go with you to a check-up. They might love the chance to hear the baby's heartbeat.
Week 14
Baby: Your
baby's ears are shifting from the neck to the sides of the head, and
the neck is getting longer and the chin more prominent. Facial features
and unique fingerprints are all there. Your baby is beginning to respond
to outside stimuli. If your abdomen is poked, the baby will try to
wriggle away.
Mom-to-be: You're probably wearing maternity clothes now. Your skin and muscles are starting to stretch to accommodate your growing baby. You may notice some constipation, because pregnancy hormones relax the bowel.
Tip of the Week: Try to ease constipation by getting moderate exercise, drinking plenty of fluids, and eating lots of fruit and vegetables.
Week 15
Baby: Your baby's body is covered by very fine hair, called lanugo, which is usually shed by birth. Eyebrows and hair on the top of the head are beginning to grow, bones are getting harder, and the baby may even be sucking his thumb.
Mom-to-be: Your uterus can probably be felt about 3 to 4 inches below your navel. Sometime in the next five weeks you'll be offered a blood test called the quadruple marker screening test to help screen for Down syndrome. You might also be offered amniocentesis, which tests a small sample of amniotic fluid withdrawn by an ultrasound-guided needle, between now and 18 weeks. You can talk with your doctor about what prenatal tests you may want.
Tip of the Week: Start learning to sleep
on your left side -- your circulation is better that way. You can try
tucking pillows behind you and between your legs. Some pregnancy pillows
support your entire body.
Week 16
Baby:
You may be able to hear the baby's heartbeat in the doctor's office.
Fine hair, lanugo, may be growing on the head. Arms and legs are moving,
and the nervous system is working.
Mom-to-be:
Within the next few weeks, you may start to feel your baby move, called
"quickening." It often feels like a gas bubble or subtle fluttering
movement. As it happens more regularly, you'll know it's your baby. Your
body is changing in many other ways. Increased blood volume to support your growing baby may produce nosebleeds,
and you may notice your leg veins are becoming more apparent. Good
news: Because your uterus is shifting, you may not have to urinate so
much.
Tip of the Week: If your leg veins bulge, you may want to wear support stockings, put your feet up when you can, and exercise to improve blood flow.
What's Happening Inside You?
Your baby's fingers and toes are well-defined; his or her eyelids, eyebrows, eyelashes, nails, and hair are formed. Teeth and bones become denser. Your baby can even suck his or her thumb, yawn, stretch and make faces.
The baby's reproductive organs and genitals are now fully developed, and your health care provider can see on ultrasound if you are having a boy or a girl. You don't have to find out the baby's sex yet -- that's up to you.
Your Pregnancy Week by Week: Weeks 17-20
FIFTH MONTH:
Week 17
Baby: Your baby now has doubled in weight in the last two weeks. Fat begins to form, helping your baby's heat production and metabolism. The lungs are beginning to exhale amniotic fluid, and the circulatory and urinary systems are working. Hair on the head, eyebrows, and eyelashes is filling in.
Mom-to-be: You're showing more now, with a typical weight gain of 5-10 pounds. You may also be noticing that your appetite has grown.
Tip of the Week:
To avoid feeling dizzy or faint, change positions slowly, especially
when you move from a lying down position to sitting or from a sitting
position to standing. If you feel lightheaded, sit down and lower your
head, or lie down for a moment.
Week 18
Baby:
Your baby's rapid growth spurt is tapering off, but reflexes are
kicking in. The baby can yawn, stretch, and make facial expressions,
even frown. Taste buds are beginning to develop and can distinguish
sweet from bitter. The baby will suck if its lips are stroked, and it
can swallow and even get the hiccups. The retinas have become sensitive to light, so if a bright light is shined on your abdomen, baby will probably move to shield its eyes.
Mom-to-be:
Your uterus, about the size of a cantaloupe, can probably be felt just
below your navel. You're most likely feeling the baby move by now. A
mid-pregnancy ultrasound may be performed between now and 22 weeks to assess the baby's growth and development and to verify the due date. If the baby is in the right position, the ultrasound may show whether it's a boy or a girl. Your heart has to work 40% to 50% harder now to support your pregnancy.
Tip of the Week: Could your partner go with you for the ultrasound? It's a chance to catch the first glimpse of your baby together.
Week 19
Baby: Your baby's skin is developing and transparent, appearing red because blood vessels are visible through it. A creamy white protective coating, called vernix, begins to develop on the baby's skin.
Mom-to-be: As your baby continues to grow, you may be feeling some mid-pregnancy aches and pains by now -- lower abdominal achiness, dizziness, heartburn, constipation, leg cramps, mild swelling of ankles and feet, and a backache. Dilated blood vessels might cause tiny, temporary red marks (called spider nevi) on your face, shoulders, and arms.
Tip of the Week: Take care of yourself! Try not to get overtired while the baby is growing so quickly.
Week 20
Baby: Your baby can hear sounds by now -- your voice, heart, and your stomach
growling, as well as sounds outside your body. The baby will cover its
ears with its hands if a loud sound is made near you, and it may even
become startled and "jump." The baby is moving often, too -- twisting,
turning, wiggling, punching and kicking.
Mom-to-be:
Congratulations! You're near the midpoint of your pregnancy. Your
uterus is just about even with your navel. Your waistline has pretty
much disappeared. Bladder infections
are more likely, because certain muscles in the urinary tract relax.
Your breathing will deepen and you may sweat more than usual because
your thyroid gland is more active.
Tip of the Week: Backache? Watch your posture. Sit with a footstool or use an ergonomic chair, avoid standing for too long, sleep with a small pillow under your side at the waist, and lift things with your legs instead of your back.
What's Happening Inside You?
Hair
is beginning to grow on your baby's head, and lanugo, a soft fine hair,
covers his or her shoulders, back, and temples. This hair protects your
baby and is usually shed at the end of the baby's first week of life.
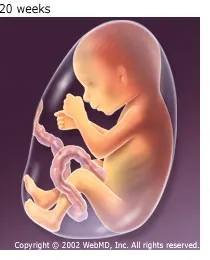
Your
baby's skin is covered with a whitish coating called vernix caseosa.
This "cheesy" substance, thought to protect baby's skin from long
exposure to the amniotic fluid, is shed just before birth.
You may begin to feel your baby move because he or she is developing muscles and exercising them. That movement is called quickening.
Your Pregnancy Week by Week: Weeks 21-25
SIXTH MONTH:
Week 21
Baby:
Your baby is steadily gaining fat to keep warm. Growth rate is slowing
down, but its organs are still maturing. Your baby's oil glands are
making a waxy film, called the vernix caseosa, that covers the skin to keep it supple in the amniotic fluid. Buds for permanent teeth are beginning to form.
Mom-to-be: You're starting to show! Your uterus is starting to extend above your navel. You've probably gained 10-14 pounds by now.
Tip of the Week: If you're interested in childbirth classes, now's a good time to start looking for one.
Week 22
Baby:
Your baby's muscles are getting stronger every week now, and the
eyelids and eyebrows are developed. Your baby moves a lot and responds
to sound, rhythm, and melody. If you sing and talk to your baby now,
those sounds may later soothe your newborn.
Mom-to-be: Your uterus is still growing, and you're probably feeling pretty good -- no more morning sickness. You may still be getting leg and foot cramps, though, and mild swelling of your ankles and feet.
Tip of the Week: To curb cramping, eat more calcium and potassium. Have a glass of milk before bedtime
or snack on potassium-rich foods, such as grapefruits, oranges, and
bananas. If you do get a leg cramp, try flexing your toes back toward
your face and keeping your leg straight.
Week 23
Baby: Your baby's skin is still wrinkled because your baby still has more weight to gain. Fine hair, called lanugo, on the body sometimes turns darker.
Mom-to-be: You've probably gained about 12-15 pounds. While pregnant,
you may notice an increase in vaginal secretions that are typically
clear-to-yellowish with a faint smell. If the color or odor changes
significantly, check in with your health care
provider to see if you have an infection. Does the small of your back
ache? Lying down, getting massages, and applying a heating pad or hot
water bottle to the area can help.
Tip of the Week: As your skin stretches, it may become dry and itchy. Keeping it moist with lotions or creams can help.
Week 24
Baby: Your baby is starting to make white blood cells,
which will help it fight off disease and infection, and may respond to
your touch or sounds. If you haven't felt the baby hiccup yet, you might
now.
Mom-to-be: Expect to gain about a pound per week this month. Your health care provider may test you for gestational diabetes between this week and 28 weeks.
Tip of the Week: Your partner might be able to hear the baby's heartbeat by putting an ear to your abdomen.
Week 25
Baby:
Your baby's skin now becomes opaque instead of transparent. The baby's
body is still covered with folds, as it needs to grow into its skin.
Heartbeat can be heard through a stethoscope or, depending on the
position of the baby, by others putting an ear against your belly.
Mom-to-be: Besides your uterus growing upward, it may be getting bigger on your abdomen's sides. You may have hemorrhoids, caused by increased blood flow, constipation, indigestion, and heartburn.
Tip of the Week: To soothe hemorrhoids, apply an ice pack or witch hazel, or try a sitz bath (soaking your bottom in shallow warm water). Over-the-counter suppositories and/or medicated wipes may also help. Don't take laxatives or mineral oil.
What's Happening Inside You?
By the end of the sixth month, your baby's finger and toe prints are visible. The eyelids begin to part and the eyes open.
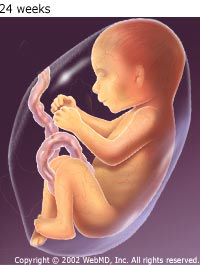
Your baby may respond to sounds by moving or increasing the pulse, and you may feel the baby hiccupping.
Second Trimester Tests During Pregnancy
Here are the prenatal tests that may be performed in the second trimester of your pregnancy:
Maternal serum alpha-fetoprotein (MSAFP) and multiple marker screening:
One or the other is offered routinely in the second trimester. This
test is an optional genetic screening test and as with all screening
tests, talk with your doctor about the pros and cons to see if it is
right for you. The MSAFP test measures the level of alpha-fetoprotein, a
protein produced by the fetus. Abnormal levels indicate the possibility (but not existence) of Down syndrome or a neural tube defect such as spina bifida, which can then be confirmed by ultrasound or amniocentesis.
When blood
drawn for the MSAFP test is also used to check levels of the hormones
estriol and hCG, it's called the triple test. When a marker called
inhibin-A is added to the screen, it is known as the quad marker. The
quad marker test significantly boosts the detection rates for Down
syndrome. The test picks up about 75% of neural tube defects and 75%-90%
of Down syndrome cases (depending on the mother's age), but many women
will have a false-positive screening. About 3% to 5% of women who have
the screening test will have an abnormal reading, but only a small
percentage of those women will actually have a child with a genetic
problem.
Ultrasounds:
Ultrasounds (sonograms) are commonly offered week 20, although they may
be done at any time during a pregnancy. A sonogram may be offered for a
variety of reasons, including verifying a due date, checking for multiple fetuses, investigating complications such as placenta previa (a low-lying placenta) or slow fetal growth, or detecting malformations like cleft palate.
Sometimes, if there are findings suspicious for a genetic abnormality
seen, you may be referred to a specialist or for further genetic
testing. During the procedure, a device is moved across the abdomen that transmits sound waves to create an image of the uterus and fetus
on a computer monitor. New three-dimensional sonograms provide an even
clearer picture of your baby, but they aren't available everywhere and
it's not clear whether they're any better than two-dimensional pictures
in contributing to a healthy pregnancy or birth.
Glucose screening: Typically done at 24 to 28 weeks, this is a routine test for pregnancy-induced diabetes,
which can result in overly large babies, difficult deliveries, and
health problems for you and your baby. This test measures your blood-sugar
level an hour after you've had a glass of a special soda. If the
reading is high, you'll take a more sensitive glucose-tolerance test, in
which you drink a glucose solution on an empty stomach and have your blood drawn every hour for 2-3 hours.
Amniocentesis:
This optional test is usually performed between 15 and 18 weeks of
pregnancy (but can be done earlier) for women who are 35 or older, have a
higher-than-usual risk of genetic disorders, or whose MSAFP or multiple
marker test results were suspicious. The procedure is done by inserting
a needle through the abdomen into the amniotic sac and withdrawing
fluid that contains fetal cells. Analysis can detect neural tube defects
and genetic disorders. The miscarriage
rate after amniocentesis varies depending on the experience of the
doctor performing the procedure, averaging about 0.2% to 0.5% at 15
weeks, but the test can detect 99% of neural tube defects and almost
100% of certain genetic abnormalities.
Fetal Doppler ultrasound:
A Doppler ultrasound test uses sound waves to evaluate blood as it
flows through a blood vessel. Fetal Doppler ultrasound can determine if
blood flow to the placenta and fetus is normal.
Fetoscopy: Fetoscopy allows a doctor to see the fetus
through a thin, flexible instrument called a fetoscope. Fetoscopy can
detect some diseases or defects that cannot be found by other tests,
such as amniocentesis, ultrasound, or chorionic villus sampling.
Because fetoscopy carries significant risks for the mother and fetus,
it is an uncommon procedure that is only recommended if there is a much
higher-than-normal chance that the baby will have an abnormality.
HEALTH CONCERNS IN SECOND TRIMESTER OF PREGNANCY:
Back Pain in Pregnancy
The good news is, your baby is growing. That's exactly what should be happening -- but it can still be tough on your back.
You've got lots of company -- most pregnant women experience back pain, usually starting in the second half of pregnancy.
You should know that there are things you can do to minimize your back pain. Here's what helps.
Causes of Back Pain in Pregnant Women
Pregnancy back pain typically happens where the pelvis meets your spine, at the sacroiliac joint.
There are many possible reasons why it happens. Here are some of the more likely causes:
- Weight gain. During a healthy pregnancy, women typically gain between 25 and 35 pounds. The spine has to support that weight. That can cause lower back pain. The weight of the growing baby and uterus also puts pressure on the blood vessels and nerves in the pelvis and back.
- Posture changes. Pregnancy shifts your center of gravity. As a result, you may gradually -- even without noticing -- begin to adjust your posture and the way you move. This may result in back pain or strain.
- Hormone changes. During pregnancy, your body makes a hormone called relaxin that allows ligaments in the pelvic area to relax and the joints to become looser in preparation for the birth process. The same hormone can cause ligaments that support the spine to loosen, leading to instability and pain.
- Muscle separation. As the uterus expands, two parallel sheets of muscles (the rectal abdominis muscles), which run from the rib cage to the pubic bone, may separate along the center seam. This separation may worsen back pain.
- Stress. Emotional stress can cause muscle tension in the back, which may be felt as back pain or back spasms. You may find that you experience an increase in back pain during stressful periods of your pregnancy.
Treatments for Back Pain in Pregnancy
More
good news: Unless you had chronic backaches before you got pregnant,
your pain will likely ease gradually before you give birth.
Meanwhile, there are many things you can do to treat low back pain or make it rarer and milder:
- Exercise. Regular exercise strengthens muscles and boosts flexibility. That can ease the stress on your spine. Safe exercises for most pregnant women include walking, swimming, and stationary cycling. Your doctor or physical therapist can recommend exercises to strengthen your back and abdomen.
- Heat and Cold. Applying heat and cold to your back may help. If your health care provider agrees, start by putting cold compresses (such as a bag of ice or frozen vegetables wrapped in a towel) on the painful area for up to 20 minutes several times a day. After two or three days, switch to heat -- put a heating pad or hot water bottle on the painful area. Be careful not to apply heat to your abdomen during pregnancy.
- Improve your posture. Slouching strains your spine. So using proper posture when working, sitting, or sleeping is a good move. For example, sleeping on your side with a pillow between the knees will take stress off your back. When sitting at a desk, place a rolled-up towel behind your back for support; rest your feet on a stack of books or stool and sit up straight, with your shoulders back. Wearing a support belt may also help.
- Counseling. If back pain is related to stress, talking to a trusted friend or counselor may be helpful.
- Acupuncture. Acupuncture is a form of Chinese medicine in which thin needles are inserted into your skin at certain locations. Studies have shown that acupuncture can be effective in relieving low back pain during pregnancy. Check with your health care provider if you're interested in trying it.
- Chiropractic. When performed correctly, chiropractic manipulation of the spine can be safe during pregnancy, but consult with your doctor before seeking chiropractic care.
- More tips:
- If you need to pick something up from the ground, use your legs to squat rather than bend over.
- Don't wear high-heeled shoes.
- Don't sleep on your back.
- Wear support hose.
If
your back pain persists, you may want to consult your doctor to see
what else you might try. Be sure to consult your doctor before taking
pain medications. Acetaminophen (Tylenol) is safe for most women to take
during pregnancy. Aspirin and other nonsteroidal anti-inflammatory
drugs (NSAIDs) such as ibuprofen (Advil, Motrin) or naproxen (Aleve) are
not advised. In some cases, your doctor may recommend other pain
medicines or muscle relaxants that are safe during pregnancy.
When to Seek Treatment From a Doctor
Back
pain, by itself, usually is not a reason to call your doctor. But you
should call your doctor right away if you experience any of the
following:
- Severe pain
- Increasingly severe pain or pain that begins abruptly
- Rhythmic cramping pains
In rare cases, severe back pain may be related to problems such as pregnancy-associated osteoporosis, vertebral osteoarthritis, or septic arthritis. Rhythmic pains may be a sign of preterm labor. So if you are experiencing any of these problems, it's important to be checked by your doctor.
Preeclampsia and Eclampsia
What Is Preeclampsia?
Formerly called toxemia, preeclampsia is a condition that pregnant women develop. It is marked by high blood pressure
and a high level of protein in the urine. Preeclamptic women will often
also have swelling in the feet, legs, and hands. This condition usually
appears during the second half of pregnancy, often in the latter part of the second or in the third trimesters, although it can occur earlier.
If
undiagnosed, preeclampsia can lead to eclampsia, a serious condition
that can put you and your baby at risk, and in rare cases, cause death.
Women with preeclampsia who have seizures are considered to have eclampsia.
There's
no way to cure preeclampsia, and that can be a scary prospect for
moms-to-be. But you can help protect yourself by learning the symptoms
of preeclampsia and by seeing your doctor for regular prenatal care.
When preeclampsia is caught early, it's easier to manage.
What Causes Preeclampsia?
The
exact causes of preeclampsia and eclampsia -- a result of a placenta
that doesn't function properly -- are not known, although some
researchers suspect poor nutrition, high body fat, or insufficient blood flow to the uterus as possible causes. Genetics plays a role, as well.
Who Is at Risk for Preeclampsia?
Preeclampsia is most often seen in first-time pregnancies, in pregnant teens, and in women over 40. Other risk factors include:
- A history of high blood pressure prior to pregnancy
- A history of preeclampsia
- Having a mother or sister who had preeclampsia
- A history of obesity
- Carrying more than one baby
- History of diabetes, kidney disease, lupus, or rheumatoid arthritis
What Are the Signs and Symptoms of Preeclampsia?
In addition to swelling, protein in the urine, and high blood pressure, preeclampsia symptoms can include:
- Rapid weight gain caused by a significant increase in bodily fluid
- Abdominal pain
- Severe headaches
- Change in reflexes
- Reduced urine or no urine output
- Dizziness
- Excessive vomiting and nausea
- Vision changes
You should seek care right away if you have:
- Sudden and new swelling in your face, hands, and eyes (some feet and ankle swelling is normal during pregnancy.)
- Blood pressure greater than 140/90.
- Sudden weight gain over 1 or 2 days
- Abdominal pain, especially in the upper right side
- Severe headaches
- A decrease in urine
- Blurry vision, flashing lights, and floaters
You
can also have preeclampsia and not have any symptoms. That's why it's
so important to see your doctor for regular blood pressure checks and
urine tests.
How Can Preeclampsia Affect My Baby and Me?
Preeclampsia can prevent the placenta from receiving enough blood, which can cause your baby to be born very small. It is also one of the leading causes of premature births, and the complications that can follow, including learning disabilities, epilepsy, cerebral palsy, hearing and vision problems.
In moms-to-be, preeclampsia can cause rare but serious complications that include:
- Stroke
- Seizure
- Water in the lungs
- Heart failure
- Reversible blindness
- Bleeding from the liver
- Bleeding after you've given birth
Preeclampsia can also cause the placenta to suddenly separate from the uterus, which is called placental abruption. This can cause stillbirth.
What Is the Treatment for Preeclampsia and Eclampsia?
The
only cure for preeclampsia and eclampsia is to deliver your baby. Your
doctor will talk with you about when to deliver based on how far along
your baby is, how well your baby is doing in your womb, and the severity
of your preeclampsia.
If your baby has developed enough, usually by 37 weeks or later, your doctor may want to induce labor or perform a cesarean section. This is will keep preeclampsia from getting worse.
If your baby is not close to term,
you and your doctor may be able to treat preeclampsia until your baby
has developed enough to be safely delivered. The closer the birth is to
your due date, the better for your baby.
If you have mild preeclampsia - also known as preclampsia with and without severe features, your doctor may prescribe:
- Bed rest either at home or in the hospital; you'll be asked to rest mostly on your left side.
- Careful observation with a fetal heart rate monitor and frequent ultrasounds
- Medicines to lower your blood pressure
- Blood and urine tests
Your doctor also may recommend that you stay in the hospital for closer monitoring. In the hospital you may be given:
- Medicine to help prevent seizures, lower your blood pressure, and prevent other problems
- Steroid injections to help your baby's lungs develop more quickly
Other treatments include:
- Magnesium can be injected into the veins to prevent eclampsia-related seizures
- Hydralazine or another antihypertensive drug to manage severe blood pressure elevations
- Monitoring fluid intake and urine output
For severe preeclampsia, your doctor may need to deliver your baby right away, even if you're not close to term.
After delivery, signs and symptoms of preeclampsia should go away within 1 to 6 weeks.
Pregnancy and Heartburn
Despite its name, heartburn has nothing to do with the heart. (Some of the symptoms, however, are similar to those of a heart attack or heart disease.) Heartburn is an irritation of the esophagus that is caused by stomach acid and is a common pregnancy complaint, especially in the third trimester when the growing uterus places pressure on the stomach.
With
gravity's help, a muscular valve called the lower esophageal sphincter,
or LES, keeps stomach acid in the stomach. The LES is located where the
esophagus meets the stomach -- below the rib cage and slightly left of
center. Normally it opens to allow food into the stomach or to permit
belching; then it closes again. But if the LES opens too often or does
not close tight enough, stomach acid can reflux, or seep, back into the
esophagus and cause a burning sensation.
Occasional heartburn isn't dangerous, but chronic heartburn can indicate serious problems, such as gastritis
or gastroesophageal reflux disease, also called GERD. Heartburn is a
daily occurrence for 10% of Americans and 50% of pregnant women. It's an
occasional nuisance for another 30% of the population.
Symptoms of Heartburn During Pregnancy
Common heartburn symptoms reported by pregnant women include:
- A burning feeling in the chest just behind the breastbone (the sternum) that occurs after eating and lasts a few minutes to several hours
- Chest pain, especially after bending over, lying down, or eating
- Burning in the throat -- or hot, sour, or salty-tasting fluid at the back of the throat
- Belching
- Chronic coughing
- Hoarseness
- Wheezing or other asthma-like symptoms
Round Ligament Pain During Pregnancy
Round ligament pain
is a sharp pain or jabbing feeling often felt in the lower belly or
groin area on one or both sides. It is one of the most common complaints
during pregnancy and is considered a normal part of pregnancy. It is most often felt during the second trimester.
Here is what you need to know about round ligament pain, including some tips to help you feel better.
Causes of Round Ligament Pain
Several
thick ligaments surround and support your womb (uterus) as it grows
during pregnancy. One of them is called the round ligament.
The
round ligament connects the front part of the womb to your groin, the
area where your legs attach to your pelvis. The round ligament normally
tightens and relaxes slowly.
As your baby and womb grow, the round ligament stretches. That makes it more likely to become strained.
Sudden
movements can cause the ligament to tighten quickly, like a rubber band
snapping. This causes a sudden and quick jabbing feeling.
Symptoms of Round Ligament Pain
Round ligament pain can be concerning and uncomfortable. But it is considered normal as your body changes during pregnancy.
The symptoms of round ligament pain include a sharp, sudden spasm in the belly. It usually affects the right side, but it may happen on both sides. The pain only lasts a few seconds.
Exercise may cause the pain, as will rapid movements such as:
Treatment of Round Ligament Pain
Here are some tips that may help reduce your discomfort:
Pain relief. Take over-the-counter acetaminophen for pain, if necessary. Ask your doctor if this is OK.
Exercise. Get plenty of exercise to keep your stomach (core) muscles strong. Doing stretching exercises or prenatal yoga can be helpful. Ask your doctor which exercises are safe for you and your baby.
A helpful exercise involves putting your hands and knees on the floor, lowering your head, and pushing your backside into the air.
Avoid sudden movements. Change positions slowly (such as standing up or sitting down) to avoid sudden movements that may cause stretching and pain.
Flex your hips. Bend and flex your hips before you cough, sneeze, or laugh to avoid pulling on the ligaments.
Apply warmth. A heating pad or warm bath may be helpful. Ask your doctor if this is OK. Extreme heat can be dangerous to the baby.
You should try to modify your daily activity level and avoid positions that may worsen the condition.
When to Call the Doctor
Always tell your doctor about any type of pain you have during pregnancy. Round ligament pain is quick and doesn't last long.
Call your health care provider immediately if you have:
- severe pain
- pain that lasts for more than a few minutes
- fever
- chills
- pain on urination
- difficulty walking
Belly
pain during pregnancy can be due to many different causes. It is
important for your doctor to rule out more serious conditions, including
pregnancy complications such as placenta abruption or non-pregnancy illnesses such as:
- inguinal hernia
- appendicitis
- stomach, liver, and kidney problems
Preterm labor pains may sometimes be mistaken for round ligament pain.
THIRD TRIMESTER(6-9 MONTHS) OF PREGNANCY:
Third Trimester of Pregnancy
Now that you've reached the third trimester, you're in the home stretch of your pregnancy. You've only got a few more weeks to go, but this part of your pregnancy can be the most challenging.
In this article, you'll learn what to expect during your third trimester of pregnancy. You'll find out which symptoms are normal, and which ones may warrant a call to your doctor.
Changes in Your Body
Backache. The extra weight
you've gained is putting added pressure on your back, making it feel
achy and sore. You might also feel discomfort in your pelvis and hips as
your ligaments loosen to prepare for labor .
To ease the pressure on your back, practice good posture. Sit up
straight and use a chair that provides good back support. At night, sleep on your side with a pillow tucked between your legs. Wear low-heeled, comfortable shoes with good arch support. To relieve back pain, use a heating pad and ask your doctor whether it's OK for you to take acetaminophen.
Bleeding. Spotting may sometimes be a sign of a serious problem, including placenta previa (the placenta grows low and covers the cervix), placental abruption (separation of the placenta from the uterine wall), or preterm labor. Call your doctor as soon as you notice any bleeding.
Braxton Hickscontractions. You might start to feel mild contractions, which are warm-ups to prepare your uterus for the real labor to come. Braxton Hicks
contractions often aren't as intense as real labor contractions, but
they may feel a lot like labor and can eventually progress to it. One
main difference is that real contractions gradually get closer and
closer together -- and more intense. If you're red in the face and out
of breath after your contractions, or they're coming regularly, call
your doctor.
Breast enlargement. By the end of your pregnancy, your breasts will have grown by as much as 2 pounds. Make sure you're wearing a supportive bra so your back doesn't suffer. Close to your due date, you may start to see a yellowish fluid leaking from your nipples. This substance, called colostrum, will nourish your baby in the first few days after birth.
Discharge. You might see more vaginal discharge
during the third trimester. If the flow is heavy enough to soak through
your panty liners, call your doctor. Close to your delivery date, you
might see a thick, clear, or slightly blood-tinged
discharge. This is your mucus plug, and it's a sign that your cervix
has begun dilating in preparation for labor. If you experience a sudden
rush of fluid, it may mean that your water has broken (although only
about 8% of pregnant women have their water break before contractions
begin). Call your doctor as soon as possible after your water breaks.
Fatigue. You might have been feeling energetic in your second trimester,
but are weary now. Carrying extra weight, waking up several times
during the night to go to the bathroom, and dealing with the anxiety of preparing for a baby can all take a toll on your energy level. Eat healthy food and get regular exercise
to give yourself a boost. When you feel tired, try to take a nap, or at
least sit down and relax for a few minutes. You need to reserve all
your strength now for when your baby arrives and you're really not getting any sleep.
Frequent urination. Now that your baby is bigger, the baby's head may be pressing down on your bladder.
That extra pressure means you'll have to go to the bathroom more
frequently -- including several times each night. You might also find
that you're leaking urine when you cough,
sneeze, laugh, or exercise. To relieve the pressure and prevent
leakage, go to the bathroom whenever you feel the urge and urinate
completely each time. Avoid drinking fluids right before bedtime
to cut down on unwanted late-night bathroom visits. Wear a panty liner
to absorb any leakage that does occur. Let your doctor know if you
experience any pain or burning with urination. These can be signs of a urinary tract infection.
Heartburn and constipation. They're caused by extra production of the hormone progesterone, which relaxes certain muscles -- including the muscles in your esophagus that normally keep food and acids down in your stomach, and the ones that move digested food through your intestines. To relieve heartburn,
try eating more frequent, smaller meals throughout the day and avoid
greasy, spicy, and acidic foods (like citrus fruits). For constipation, increase your fiber intake and drink extra fluids to keep things moving more smoothly. If your heartburn or constipation is really bothering you, talk to your doctor about what medications may be safe for you to take for symptom relief.
Hemorrhoids.Hemorrhoids are actually varicose veins -- swollen veins that form around the anus. These veins enlarge during pregnancy because extra blood
is flowing through them and the weight of pregnancy increases the
amount of pressure to the area. To relieve the itch and discomfort, try
sitting in a warm tub or sitz bath. Ask your doctor whether you can also try an over-the-counter hemorrhoid ointment or stool softener.
Shortness of breath. As your uterus expands, it rises up until it sits just under your rib cage, leaving less room for your lungs to expand. That added pressure on your lungs can make it more difficult to breathe. Exercising can help with shortness of breath. You can also try propping up your head and shoulders with pillows while you sleep.
Spider and varicose veins.
Your circulation has increased to send extra blood to your growing
baby. That excess blood flow can cause tiny red veins, known as spider
veins, to appear on your skin.
Spider veins may get worse in your third trimester, but they should
fade once your baby is born. Pressure on your legs from your growing
baby may also cause some surface veins in your legs to become swollen
and blue or purple. These are called varicose veins. Although there's no
way to avoid varicose veins, you can prevent them from getting worse
by:
- Getting up and moving throughout the day
- Wearing support hose
- Propping up your legs whenever you have to sit for long periods of time.
Varicose veins should improve within a few months after you deliver.
Swelling. Your rings might be feeling tighter these days, and you may also notice that your ankles and face are looking bloated. Mild swelling is the result of excess fluid retention (edema). To reduce swelling, put your feet
up on a stool or box whenever you sit for any length of time, and
elevate your feet while you sleep. If you have sudden onset of swelling
though, seek medical attention immediately as it may be a sign of preeclampsia, a dangerous pregnancy complication.
Weight gain.
Aim for a weight gain of 1/2 pound to 1 pound a week during your third
trimester. By the end of your pregnancy, you should have put on a total
of about 25 to 35 pounds (your doctor may have recommended that you gain
more or less weight if you started out your pregnancy underweight or overweight). The extra pounds you've put on are made up of the baby's weight, plus the placenta, amniotic fluid,
increased blood and fluid volume, and added breast tissue. If your baby
seems to be too small or too big based on the size of your belly, your
doctor will do an ultrasound to check his growth.
Red Flag Symptoms
Any of
these symptoms could be a sign that something is wrong with your
pregnancy. Don't wait for your regular prenatal visit to talk about it.
Call your doctor right away if you experience:
- Severe abdominal pain or cramps
- Severe nausea or vomiting
- Bleeding
- Severe dizziness
- Pain or burning during urination
- Rapid weight gain (more than 6.5 pounds per month) or too little weight gain.
Your Pregnancy Week by Week: Weeks 26-30
SEVENTH MONTH:
Week 26
Baby: Your baby's hearing is fully developed. As the baby reacts to sounds, its pulse increases.Your baby will even move in rhythm to music. Lungs are still growing but are not yet mature. Patterns of your baby's brain waves appear like a full-term newborn. He or she also has patterns of sleeping and waking.
Mom-to-be: The baby's constant movements should be reassuring. You'll be putting on weight
at the rate of about 1 pound per week now. You may be feeling some rib
pain as your baby grows and pushes upward on your rib cage. The pressure
may also be causing indigestion and heartburn. You may also feel stitch-like pains down the sides of your abdomen as your uterine muscle stretches.
Tip of the Week: If you're planning to return to work, you might want to begin checking out child care
in your area. Nannies cost about $250 to $600 per week, group day care
typically ranges from $125 to $200 per week, and home day care runs from
about $75 to $125 per week. Stay open-minded about various child care
arrangements.
Week 27
Baby:Your baby's hands are active. Thumb-sucking calms the baby and strengthens cheek and jaw muscles. Your baby can cry now.
Mom-to-be: You may see stretch marks
as your uterus continues to expand. Most women have gained about 16 to
22 pounds by now. Your balance and mobility also may be changing as you
grow larger.
Tip of the Week: During your last trimester, you should talk to your doctor or midwife about the delivery. They can let you know about signs to predict labor and how far apart the contractions
should be before going to the hospital or birth center. It's also the
time to begin interviewing pediatricians and to take care of other
logistics, like pre-registration at the place where you'll give birth and a birthing plan (what you envision your labor and delivery will be like). This plan should be written in your patient record or attached to it in the form of a birth plan.
Week 28
Baby: Your
baby measures about 10 inches from crown to rump, or a total length of
about 15.75 inches from head to toe, and weighs about 2.4 pounds. Brain waves show rapid eye movement (REM) sleep, which means your baby may be dreaming. Eyelids are opening. Branches of lungs are developing.
Mom-to-be: Your uterus extends well above your navel. As the baby gets bigger and stronger this month, you may be experiencing leg cramps and mild swelling of ankles and feet, difficulty sleeping, shortness of breath, lower abdominal achiness, clumsiness, or scattered Braxton Hicks
contractions (hardening and relaxing of the uterus, like a rehearsal
for labor). You may also be urinating more frequently again as the
uterus continues to push on your bladder.
Tip of the Week:
Even if your partner is planning on being with you in the delivery
room, you might want to consider hiring a doula -- a professional labor
assistant who provides support, but not medical aid, for the mother and
her partner. Studies show that doulas can shorten a woman's labor and
reduce the likelihood of needing pain medication, forceps or vacuum deliveries, or a cesarean section.
Week 29
Baby: Your baby's eyes
are almost always blue and can distinguish bright sunlight or
artificial light through the uterine wall. The baby is performing fewer
acrobatics as conditions in the womb become more cramped, but he's still
doing a lot of kicking and stretching.
Mom-to-be: You've probably gained 19-25 pounds. You still have some time to go, so you may want to remind yourself of signs of premature labor, including menstrual-like cramps or lower back pain, a trickle of amniotic fluid, or a watery pinkish or brownish discharge preceded sometimes by the passage of a thick, gelatinous mucus plug. Tell your health care provider ASAP if that happens -- they can sometimes stop labor from progressing with bed rest, medications, and possibly also hospitalization.
Tip of the Week: Your blood pressure typically may rise a little around the seventh month. Tell your health care provider if you get severe headaches; blurred vision; severe swelling of hands, feet, or ankles; or if you gain a lot of weight. These symptoms could signal the beginning of preeclampsia, a dangerous condition marked by high blood pressure and high levels of protein in the urine during pregnancy.
Baby: Your baby measures about 17 inches from
head to toe and weighs about 3 pounds. Baby is growing plumper and
beginning to control its own body temperature. Eyebrows and eyelashes are fully developed, and hair on the head is getting thicker. Head and body are now proportioned like a newborn's. Hands are now fully formed and fingernails are growing.
Mom-to-be: Your uterus is about 4 inches above your navel, and it may be hard to believe you
still have about 10 weeks to go as the baby continues to push on your
ribs. You may be feeling more discomfort in your pelvis and abdomen.
You'll probably be gaining about a pound a week.
Tip of the Week:
The membranes around the baby that contain the amniotic fluid are
called the bag of water. They usually do not break until just before the
onset of labor, but if they break prematurely, an infection becomes
more likely, so call your health care provider immediately.
What's Happening Inside You?
Your
baby changes position frequently and responds to stimuli, including
sound, pain, and light. At the end of the seventh month, fat begins to
be deposited on your baby.
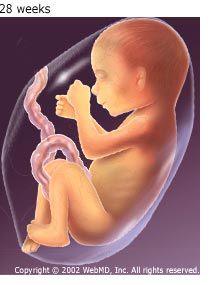
The amniotic fluid begins to diminish.
Your Pregnancy Week by Week: Weeks 31-34
EIGHT MONTH:
Week 31
Baby: Your baby can hear distinct sounds, including familiar voices and music.
Mom-to-be: Your uterus now fills a large part of your abdomen, and you've probably gained 21-27 pounds. You're probably anticipating the birth -- it won't be long now.
Tip of the Week: Practice your breathing and relaxation exercises.
Week 32
Baby:
Your baby measures about 18.9 inches long from head to toe and weighs
almost 4 pounds. Baby fills almost all the space in your uterus now, but
may still have enough room to do somersaults. A layer of fat is forming
under your baby's skin. The baby is practicing opening his eyes and breathing.
Mom-to-be:
You'll probably start seeing your practitioner every two weeks until
the last month, when you'll likely switch to weekly visits. You may
continue to get backaches and leg cramps. You may also notice a yellowish fluid, called colostrum, leaking from your breasts -- it comes before milk production.
Tip of the Week: You might be carrying differently from others at the same stage of pregnancy.
Whether you're carrying higher or lower, bigger or smaller, wider or
more compact depends on the size and position of the baby, your body
type, and how much weight
you've gained. For more comfort, drink plenty of fluids, elevate your
legs when sitting, lie on your left side, and wear support stockings.
Week 33
Baby:
The next few weeks will mark lots of growth in the baby. The baby will
gain more than half its birth weight in the next seven weeks. Your baby
begins to move less now as it runs out of room and curls up with knees bent, chin resting on chest, and arms and legs crossed.
Mom-to-be:You've gained 22-28 pounds by now. Of the pound a week you're gaining now, roughly half is going to your baby.
Tip of the Week: It's safe to keep having sex with your partner, though you may be too uncomfortable. Talk with your partner about other ways to remain intimate, including back rubs and foot massages.
Week 34
Baby: Your
baby measures about 19.8 inches from head to toe and weighs about 5
pounds. The baby is probably settling into the head-down position,
although it might not be final. Organs are now almost fully mature,
except for lungs, and the skin is pink instead of red. Fingernails reach the ends of fingers, but toenails are not yet fully grown. The baby might have lots of hair and may not move as often, due to the tight fit.
Mom-to-be: Your uterus hardens and contracts as practice for labor, known as Braxton Hickscontractions,
but you may not feel them yet. Your pelvis has expanded and may ache,
especially at the back. The uterus is pushed hard against your lower
ribs and your rib cage may be sore, and your navel is probably pushing
out as a result of your abdomen being stretched.
Tip of the Week: Start thinking about whether you want to try breastfeeding. You may want to consult a lactation expert or simply talk with friends or relatives who can share their experiences.
What's Happening Inside You?
By
the end of these four weeks, your baby will weigh as much as 5 pounds.
Your baby continues to mature and develop reserves of body fat. You may
notice that your baby is kicking more. The baby's brain
is developing rapidly at this time, and he or she can hear. Most
internal systems are well developed, but the lungs may still be
immature.
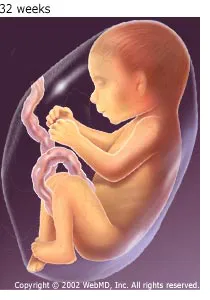
Your Pregnancy Week by Week: Weeks 35-40
NINTH MONTH:
Week 35
Baby: Your baby's lungs are almost fully developed. It's still building fat deposits beneath its skin to keep warm after it leaves your womb.
Mom-to-be:
Your uterus is about 6 inches above your navel. By now, you've probably
gained 24-29 pounds. Your doctor will test you for Group B streptococcus bacteria between now and 37 weeks.
Tip of the Week: Are you ready for the baby? Be sure you've collected the necessary baby clothes, equipment -- especially a car seat -- and furniture to get you through the first few weeks, at least, after your baby is born.
Week 36
Baby: Your baby measures about 20.7 inches from head to toe and weighs about 6 pounds. The baby may drop lower in your abdomen, usually assuming the head-down position to prepare for birth. The brain has been developing rapidly, and your baby is practicing blinking.
Mom-to-be:
Your uterus has grown bigger these last few weeks and is probably up
under your ribs. But you're in the home stretch! After this week, you'll
see your doctor weekly. You may switch between fatigue and extra bursts of energy. You may also have an achier back and feel heaviness and discomfort in your buttocks and pelvis.
Tip of the Week:
Start stocking your freezer with foods that can be easily popped into
the oven or microwave after you bring your baby home. Chili, casseroles,
and other simple dishes can be prepared and frozen ahead of time for
use later.
Week 37
Baby:
Your baby is about 21 inches from head to toe and weighs almost 6.5
pounds. The baby is getting rounder every day, and skin is getting
pinker and losing its wrinkly appearance. Your baby's head is usually
positioned down into the pelvis by now.
Mom-to-be: Your uterus may stay the same size as it was for the last week or two. Your weight gain should be about as high as it will go, about 25 to 35 pounds. About this time, your doctor might perform a pelvic exam to check on the progress of your pregnancy.
Tip of the Week:
Just in case you deliver early, consider packing two bags for the
hospital. Pack one bag for you, with warm socks, a robe, lip balm, and
everything you'll want during labor. Pack the other bag with the items
you'll want for your newborn.
Week 38
Baby: Most of your baby's downy hair,
lanugo, and whitish coating, vernix, are disappearing. Your baby is
getting its antibodies from you to protect against illness. The baby's
growth is slowing, but fat cells under skin get plumper for life outside
the womb. Your baby is almost ready for birth.
Mom-to-be:
You're probably not getting any bigger, but you may be feeling more
uncomfortable. Make sure you have a bag packed for when you deliver. It won't be long now -- 95% of all babies are born within two weeks of their mother's due date.
Tip of the Week: You may want to consider whether you'll circumcise your baby if it's a boy. Circumcision isn't as much a medical issue as a cultural or religious one.
Week 39
Baby: Your baby's arm and leg muscles are strong, and toenails and fingernails are in place. The baby's head has dropped into the mother's pelvis -- a head-down position lets you breathe a little easier.
Mom-to-be:
You're probably feeling quite large and uncomfortable. Your uterus has
filled your pelvis and most of your abdomen, pushing everything else out
of the way. Your center of gravity has shifted, so you may feel
clumsier than usual.
Tip of the Week: Watch for signs of labor, but don't get too obsessed. It could happen soon or still be a week away. Some differences between false labor and contractions:
False labor pains usually concentrate in the lower abdomen and groin,
while true labor pains may start in the lower back and may spread
through the entire abdomen. Real labor also becomes stronger and more
powerful as time passes.
Week 40
Baby:
Boys often tend to weigh a little more than girls. More lanugo falls
out, but some may remain at birth on the baby's shoulders, folds of
skin, and backs of ears.
Mom-to-be: It's
almost time! Birth should happen soon now, but don't worry if your due
date comes and goes. Only 5% of all babies are born exactly on the
predicted due date. It may be more difficult for you to get a good
night's sleep, because it's hard to find a comfortable position. Still, try to rest as much as possible, with your feet up if you can.
Tip of the Week: If you think you're in labor, don't eat. Even something light in your stomach can cause nausea.
What's Happening Inside You?
Your
baby continues to grow and mature. The lungs are nearly fully
developed. Your baby's reflexes are coordinated so he or she can blink,
close the eyes, turn the head, grasp firmly, and respond to sounds, light, and touch.
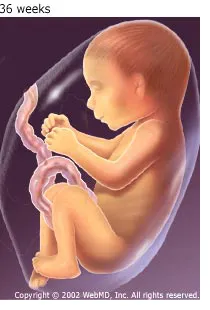
You
should still feel movement every day. Your baby's position changes to
prepare itself for labor and delivery. The baby drops down in your
pelvis, and usually his or her head is facing down toward the birth
canal.
Third Trimester Tests During Pregnancy
These tests are common in the third trimester of pregnancy:
Group B streptococcus screening: Vaginal and rectal swabs are taken at 35 to 37 weeks of pregnancy to detect group B strep bacteria. Although group B strep can be present in up to 30% of all healthy women, it's the leading cause of life-threatening infections in newborns and can also cause mental retardation, impaired vision, and hearing loss. Women who test positive are treated with antibiotics during delivery to protect the baby from contracting the infection at birth. As an alternative, your physician or midwife may choose not to test for strep but to treat you in labor if certain risk factors develop.
Electronic fetal heart monitoring: Electronic fetal heart monitoring is done during pregnancy, labor, and delivery to monitor the heart rate of the fetus. The fetal heart rate can indicate whether the fetus is doing well or is in trouble and can be done any time after 20 weeks.
Nonstress test: Done weekly in many high-risk pregnancies, such as in cases where a women is carrying more than one fetus, or has diabetes or high blood pressure, this test involves using a fetal monitor strapped across the mother's abdomen to measure the baby's heart rate as it moves. It's also used for monitoring overdue babies.
Contraction stress test: Also done in high-risk pregnancies, a fetal monitor measures the baby's heart rate in response to contractions
stimulated either by oxytocin (Pitocin) or nipple stimulation. Doctors
use the measurements to predict how well the baby will cope with the
stress of labor.
Biophysical profile: Combines a nonstress test with an ultrasound for a more accurate evaluation of the baby.
HEALTH CONCERN IN THIRD TRIMESTER OF PREGNANCY:
Braxton Hicks or True Labor Contractions?
Before "true" labor begins, you may have "false" labor pains. These are also known as Braxton Hickscontractions.
They are your body's way of getting ready for the real thing -- the day
you give birth -- but they are not a sign that labor has begun or is
getting ready to begin.
What Do Braxton Hicks Contractions Feel Like?
Some women describe Braxton Hicks contractions as tightening in the abdomen that comes and goes. Many women say these “false” contractions feel like mild menstrual cramps. Braxton Hicks contractions may be uncomfortable, but they do not cause labor or open the cervix.
Unlike true labor, Braxton Hicks contractions:
- Are usually not painful
- Don’t happen at regular intervals
- Don’t get closer together
- Don’t increase when you walk
- Do not last longer as they go on
- Do not feel stronger over time
You may feel Braxton Hicks contractions during the third trimester or as early as your second trimester. They are perfectly normal and nothing to worry about.
If you’re having Braxton Hicks contractions, you really don't need to do anything. If they’re making you uncomfortable:
- Take a walk. False labor contractions often stop when you change position or get up and move.
- Get some sleep or rest.
- Relax by taking a warm bath or by listening to music.
- Get a massage.
Abdominal Pain That’s Not Labor
Sharp, shooting pains on the sides of your abdomen are called round ligament pain.
The pain is from the ligaments that support your uterus and attach to
your pelvis -- they’re being stretched as your uterus grows. The pain
may also travel into your groin.
Round ligament pain tends to occur with movement, like standing up, rolling over, coughing, sneezing, or even urinating. It typically only lasts a few seconds or minutes.
To ease the discomfort in your sides:
- Try changing your position or activity. Lying on your opposite side may help.
- Support your abdomen when you stand or roll over. Move more slowly.
- Try to rest. A hot bath or heating pad may help.
What Do True Labor Contractions Feel Like?
True labor feels different for every woman. It may even feel different from one pregnancy to the next.
Labor contractions cause pain
and pressure in your pelvis and discomfort or a dull ache in your back
or lower abdomen. Some women may also feel pain in their sides and
thighs. The pain comes and goes at regular intervals and increases in
frequency and intensity with time.
Some women describe contractions as strong menstrual cramps, while others describe them as strong waves that feel like diarrhea cramps.
If you have signs of true labor, call your doctor or midwife immediately. If you're not sure, call your health care provider anyway. If you have any of the following symptoms, you may be in true labor.
- Contractions every 10 minutes or more than five contractions in an hour
- Regular tightening or pain in your back or lower abdomen
- Increasing pressure in your pelvis or vagina
- Vaginal bleeding
- Fluid leaking from your vagina
- Flu-like symptoms such as nausea, vomiting, or diarrhea
How Do Braxton Hicks Compare to True Labor Contractions?
To
figure out if the contractions you are feeling are the real thing and
you're going into labor, ask yourself the following questions.
How often do the contractions happen?
- False Labor: Contractions are often irregular and don’t get closer together.
- True Labor: Contractions come at regular intervals and last about 30-70 seconds. As time goes on, they get closer together and stronger.
Do they change when you move?
- False Labor: Contractions may stop when you walk or rest, or may even stop if you change positions.
- True Labor: Contractions continue despite how you move or change positions. They also continue when you try to rest.
How strong are they?
- False Labor: Contractions are usually weak and don't get much stronger. Or they may be strong at first and then get weaker.
- True Labor: Contractions get steadily stronger and stronger.
Where do you feel the pain?
- False Labor: You usually feel it only in the front of your abdomen or pelvis.
- True Labor: Contractions are more intense and may start in your lower back and move to the front of your abdomen. Or they may start in your abdomen and move to your back.
Hate to Bother My Health Care Provider With 'False Alarms.' When Should I Call?
Talk
to your doctor early in pregnancy about what may or may not be normal
and reasons you should call. (This is very important!)
If
you're not sure what you're feeling may be labor, call your doctor or
midwife. They should be available any time to answer questions and to
discuss your concerns about whether or not your contractions are signs
of true labor. Don't be afraid to call. Your doctor or midwife will ask
you some questions and may want you to be evaluated.
Absolutely call your doctor or midwife right away, at any time, if you have:
- Any vaginal bleeding
- Continuous leaking of fluid, or if your water breaks (can be a gushing or a trickling of fluid)
- Strong contractions every 5 minutes for an hour
- Contractions that you are unable to "walk through"
- A noticeable change in your baby's movement, or if you feel less than 10 movements every 2 hours
- Any symptoms of true labor contractions if you are not yet 37 weeks.
Methods of Childbirth
Vaginal delivery is the most common and safest type of childbirth.
When necessary in certain circumstances, forceps (instruments
resembling large spoons) may be used to cup your baby's head and help
guide the baby through the birth canal. Vacuum delivery is another way
to assist delivery and is similar to forceps delivery. In vacuum
delivery, a plastic cup is applied to the baby's head by suction and the
health care provider gently pulls the baby from the birth canal.
Vaginal delivery
may not always be possible. Caesarean delivery (C-section) may be
necessary for the safety of you and your baby, especially if one of
these complications is present:
- Your baby is not in the head-down position.
- Your baby is too large to pass through the pelvis.
- Your baby is in distress.
Most often, the need for a cesarean delivery is not determined until after labor
begins. Once a woman has had a cesarean delivery, future deliveries are
often also done by cesarean. That's because surgery done on the uterus
increases the risk of it rupturing during a future vaginal delivery.
Prolonged Labor
Childbirth
is a unique experience for every woman, whether you're a first-time mom
or a longtime parent. Sometimes, the baby comes really fast. Other
times, well, not so fast. How quickly your bundle of joy arrives depends
on many things, including how fast something called labor is happening.
Labor is a series of intense, repeated muscle contractions. The contractions help push the baby out of the uterus (womb) and into the birth canal.
You
will probably feel the contractions in the lower back and belly area.
This is called labor pains. The contractions help dilate (widen) the
opening to the vagina (called the cervix). This allows the baby to move out of your body and be born.
First-time
moms are usually in labor for about 12 to 18 hours, on average. If
you've had a baby before, labor usually goes more quickly, usually about
half that amount of time.
What Is Prolonged Labor?
Sometimes, labor stalls or occurs much too slowly. Prolonged labor may also be referred to as "failure to progress."
Prolonged
labor can be determined by labor stage and whether the cervix has
thinned and opened appropriately during labor. If your baby is not born
after approximately 20 hours of regular contractions, you are likely to
be in prolonged labor. Some health experts may say it occurs after 18 to
24 hours.
If you are carrying twins or more, prolonged labor is labor that lasts more than 16 hours.
Your doctor may refer to slow labor as "prolonged latent labor."
Prolonged labor may happen if:
- The baby is very big and cannot move through the birth canal.
- The baby is in an abnormal position. Normally, the baby is head-down facing your back.
- The birth canal is too small for the baby to move through.
- Your contractions are very weak.
What Happens if Labor Goes Too Slowly?
Most women dream
of a fast labor and swift delivery. But if your labor seems to be going
very slowly, take comfort in knowing that your doctor, nurse, or midwife will closely monitor you and your baby for any problems during this time.
he medical team will check:
- How often you have contractions.
- The strength of your contractions.
The following tests will be done:
- Intrauterine Pressure Catheter Placement (IUPC) - a tiny straw monitor is placed into the womb beside the baby that not only lets your doctor know when a contraction is occurring, but how strong the contractions are. If your doctor does not feel like the contractions are strong enough, at this point is when they may consider adding pitcoin.
- Continuous electronic fetal monitoring (EFM) to measure the baby's heart rate.
How Is Prolonged Labor Treated?
If
your labor is going slowly, you may be advised to just rest for a
little while. Sometimes medicine is given to ease your labor pains and
help you relax. You may feel like changing your body position to become
more comfortable.
Additional treatment depends on why your labor is going slowly.
If
the baby is already in the birth canal, the doctor or midwife may use
special tools called forceps or a vacuum device to help pull the baby
out through the vagina.
If
your doctor feels like you need more or stronger contractions, you may
receive Pitocin (oxytocin). This medicine speeds up contractions and
makes them stronger. If after your doctor feels like you are contracting
enough and the labor is still stalled, you may need a C-section.
If the baby is too big, or the medicine does not speed up delivery, you will need a C-section.
Risks of Prolonged Labor
Prolonged labor increases the chances that you will need a C-section.
Labor that takes too long can be dangerous to the baby. It may cause:
- low oxygen levels for the baby
- abnormal heart rhythm in the baby
- abnormal substances in the amniotic fluid
- uterine infection
If
the baby is in distress, you will need an emergency delivery. This is
the time where close monitoring is important to the health of you and
your baby.
Normal Labor and Delivery Process
After months of anticipation, your baby's due date is near. Here's what you can expect from the start of labor until the first days and weeks with your new baby.
Signs of Labor
No
one can predict with certainty when labor will begin -- the due date
your doctor gives you is merely a point of reference. It is normal for
labor to start as early as three weeks before that date or as late as
two weeks after it. The following are signs that labor is probably not
far away:
- Lightening. This occurs when your baby's head drops down into your pelvis in preparation for delivery. Your belly may look lower and you may find it easier to breathe as your baby no longer crowds your lungs. You may also feel an increased need to urinate, because your baby is pressing on your bladder. This can occur a few weeks to a few hours from the onset of labor.
- Bloody show. A blood-tinged or brownish discharge from your cervix is the released mucus plug that has sealed off the womb from infection. This can occur days before or at the onset of labor.
- Diarrhea. Frequent loose stools may mean labor is imminent.
- Ruptured membranes. Fluid gushing or leaking from the vagina means the membranes of the amniotic sac that surrounded and protected your baby have ruptured. This can occur hours before labor starts or during labor. Most women go into labor within 24 hours. If labor does not occur naturally during this time frame, doctors may induce labor to prevent infections and delivery complications.
- Contractions. Although it's not unusual to experience periodic, irregular contractions (uterine muscle spasms) as your labor nears, contractions that occur at intervals of less than 10 minutes are usually an indication that labor has begun.
Stages of Labor
Labor is typically divided into three stages:
The
first, the latent phase, is the longest and least intense. During this
phase, contractions become more frequent, helping your cervix to dilate
so your baby can pass through the birth canal. Discomfort at this stage
is still minimal. During this phase, your cervix will begin to dilate
and efface, or thin out. If your contractions are regular, you will
probably be admitted to the hospital during this stage and have frequent
pelvic exams to determine how much the cervix is dilated.
During the active phase, the cervix begins to dilate more rapidly. You may feel intense pain or pressure in your back or abdomen
during each contraction. You may also feel the urge to push or bear
down, but your doctor will ask you to wait until your cervix is
completely open.
During transition, the cervix fully
dilates to 10 centimeters. Contractions are very strong, painful, and
frequent, coming every three to four minutes and lasting from 60 to 90
seconds.
Stage 2.
Stage 2 begins when the cervix is completely opened. At this point, your doctor will give you the OK to push. Your pushing, along with the force of your contractions, will propel your baby through the birth canal. The fontanels (soft spots) on your baby's head allow it to fit through the narrow canal.
Your
baby's head crowns when the widest part of it reaches the vaginal
opening. As soon as your baby's head comes out, your doctor will suction
amniotic fluid, blood, and mucus from his or her nose and mouth. You will continue to push to help deliver the baby's shoulders and body.
Once your baby is delivered, your doctor -- or your partner, if he has requested to do so -- clamps and cuts the umbilical cord.
Stage 3.
After your baby is delivered, you enter the final stage of labor. In this stage, you deliver the placenta, the organ that nourished your baby inside the womb.
Each woman and each labor is different. The amount of time spent in each stage of delivery will vary. If this is your first pregnancy, labor and delivery usually lasts about 12 to 14 hours. The process is usually shorter for subsequent pregnancies.
Pain Treatments
Just as the amount of time in labor varies, the amount of pain women experience is different, too.
The
position and size of your baby and strength of your contractions can
influence pain, as well. Although some women can manage their pain with
breathing and relaxation techniques learned in childbirth classes, others will need other methods to control their pain.
Some of the more commonly used pain-relief methods include:
Medications. Several
drugs are used to help ease the pain of labor and delivery. Although
these drugs are generally safe for the mother and baby, as with any
drugs, they have the potential for side effects.
Pain-relieving drugs fall into two categories: analgesics and anesthetics.
Analgesics
relieve pain without the total loss of feeling or muscle movement.
During labor, they may be given systemically by injection into a muscle
or vein or regionally by injection into the lower back to numb your
lower body. A single injection into the spinal fluid that relieves pain
quickly is referred to as a spinal block. An epidural
block continuously administers pain medication to the area around your
spinal cord and spinal nerves through a catheter inserted into the
epidural space. Possible risks of both include decreased blood pressure, which can slow the baby's heart rate, and headache.
Anesthetics
block all feeling, including pain. They also block muscle movement.
General anesthetics cause you to lose consciousness. If you have a
cesarean delivery, you may be given general, spinal, or epidural
anesthesia. The appropriate form of anesthesia will depend on your
health, your baby's health, and the medical conditions surrounding your delivery.
Non-Drug Options. Non-drug methods for relieving pain include acupuncture,
hypnosis, relaxation techniques, and changing position frequently
during labor. Even if you choose non-drug pain relief, you can still ask
for pain medications at any point during your delivery.
What to Expect After Delivery
Just as your body went through many changes before birth, it will go through transitions as you recover from childbirth.
Physically you may experience the following:
- Pain at the site of the episiotomy or laceration. An episiotomy is a cut made by your doctor in the perineum (the area between the vagina and the anus) to help deliver the baby or prevent tearing. If this was done, or the area was torn during birth, the stitches may make walking or sitting difficult. It also can be painful when you cough or sneeze during the healing time.
- Sore breasts. Your breasts may be swollen, hard, and painful for several days as your milk comes in. Your nipples may also be sore.
- Hemorrhoids.Hemorrhoids (swollen varicose veins in the anal area) are common after pregnancy and delivery.
- Constipation. Having a bowel movement may be difficult for a few days after delivery. Hemorrhoids, episiotomies, and sore muscles can cause pain with bowel movements.
- Hot and cold flashes. Your body's adjustment to changing levels of hormones and blood flow can cause you to perspire one minute and reach for a blanket to cover yourself the next.
- Urinary or fecal incontinence. Muscles stretched during delivery, particularly after a long labor, may cause you to leak urine when you laugh or sneeze or may make it difficult to control bowel movements, causing accidental bowel leakage.
- "After pains." After giving birth, you will continue to experience contractions for a few days as your uterus returns to its pre-pregnancy size. You may notice contractions most while your baby is nursing.
- Vaginal discharge(lochia). Immediately following birth you will experience a bloody discharge heavier than a regular period. Over time, the discharge will fade to white or yellow and then stop entirely within two months.
Emotionally you may experience irritability, sadness, or
crying, commonly referred to as the "baby blues," in the days or weeks
after delivery. These symptoms occur in up to 80% of new mothers and may
be related to physical changes (including hormone changes and
exhaustion) and your emotional adjustment to the responsibilities of
caring for a newborn.
If these problems persist, inform your doctor or other health professional; you could be experiencing postpartum depression, a more serious problem that affects between 10% and 25% of new mothers.
What is a cesarean section?
A cesarean section is
the delivery of a baby through a cut (incision) in the mother's belly and
uterus. It is often called a C-section. In most cases,
a woman can be awake during the birth and be with her newborn soon afterward.
See a picture of a
delivery by C-section .
.
 .
.
If you are pregnant, chances are good that
you will be able to deliver your baby through the birth canal (vaginal birth).
But there are cases when a C-section is needed for the safety of the mother or
baby. So even if you plan on a vaginal birth, it's a good idea to learn about
C-section, in case the unexpected happens.
When is a C-section needed?
A C-section may be planned or unplanned. In most cases, doctors do cesarean sections because of problems that arise during labor. Reasons you might need an unplanned C-section include:
- Labor is slow and hard or stops completely.
- The baby shows signs of distress, such as a very fast or slow heart rate.
- A problem with the placenta or umbilical cord puts the baby at risk.
- The baby is too big to be delivered vaginally.
When doctors know about a problem ahead of time, they may
schedule a C-section. Reasons you might have a planned C-section
include:
- The baby is not in a head-down position close to your due date.
- You have a problem such as heart disease that could be made worse by the stress of labor.
- You have an infection that you could pass to the baby during a vaginal birth.
- You are carrying more than one baby (multiple pregnancy).
- You had a C-section before, and you have the same problems this time or your doctor thinks labor might cause your scar to tear (uterine rupture).
In some cases, a woman who had a C-section in the past
may be able to deliver her next baby through the birth canal. This is called
vaginal birth after cesarean (VBAC). If you have had a
previous C-section, ask your doctor if VBAC might be an option this time.
In the past 40 years, the rate of cesarean deliveries has jumped
from about 1 out of 20 births to about 1 out of 3 births.1 This trend has caused experts to worry that C-section is
being done more often than it is needed. Because of the risks, experts feel
that C-section should only be done for medical reasons.
Most mothers and
babies do well after C-section. But it is major surgery, so it carries more
risk than a normal vaginal delivery. Some possible risks of C-section
include:
- Infection of the incision or the uterus.
- Heavy blood loss.
- Blood clots in the mother's legs or lungs.
- Injury to the mother or baby.
- Problems from the anesthesia, such as nausea, vomiting, and severe headache.
- Breathing problems in the baby if it was delivered before its due date.
If she gets pregnant again, a woman with a C-section scar
has a small risk of the scar tearing open during labor (uterine rupture). She
also has a slightly higher risk of a problem with the
placenta, such as
placenta previa.
How is a C-section done?
Before a C-section, a
needle called an
IV is put in one of the mother's veins to give fluids
and medicine (if needed) during the surgery. She will then get medicine (either
epidural or
spinal anesthesia) to numb her belly and legs.
Fast-acting
general anesthesia, which makes the mother sleep
during the surgery, is only used in an emergency.
After the
anesthesia is working, the doctor makes the incision. Usually it is made low
across the belly, just above the pubic hair line. This may be called a "bikini
cut." Sometimes the incision is made from the navel down to the pubic area. See
a picture of
C-section incisions . After lifting the baby out, the doctor removes the placenta
and closes the incision with stitches.
. After lifting the baby out, the doctor removes the placenta
and closes the incision with stitches.
 . After lifting the baby out, the doctor removes the placenta
and closes the incision with stitches.
. After lifting the baby out, the doctor removes the placenta
and closes the incision with stitches.How long does it take to recover from a C-section?
Most women go home 3 to 5 days after a C-section, but it may take 4 weeks
or longer to fully recover. By contrast, women who deliver vaginally usually go
home in a day or two and are back to their normal activities in 1 to 2 weeks.
Before you go home, a nurse will tell you how to care for the
incision, what to expect during recovery, and when to call the doctor. In
general, if you have a C-section:
- You will need to take it easy while the incision heals. Avoid heavy lifting, intense exercise, and sit-ups. Ask family members or friends for help with housework, cooking, and shopping.
- You will have pain in your lower belly and may need pain medicine for 1 to 2 weeks.
- You can expect some vaginal bleeding for several weeks. (Use sanitary pads, not tampons.)
Pregnancy and the Stages of Labor and Childbirth:
Pregnancy
labor happens in three stages and lasts on average 12 to 24 hours for a
first birth. Usually, labor is shorter for subsequent births.
The First Stage of Labor
The first stage is the longest part of labor and can last up to 20 hours. It begins when your cervix
starts to open (dilate) and ends when it is completely open (fully
dilated) at 10 centimeters. When the cervix dilates from 0 to 3 or 4
centimeters, contractions get stronger as time progresses. Mild contractions
begin at 15 to 20 minutes apart and last 60 to 90 seconds. The
contractions become more regular until they are less than 5 minutes
apart. This part of labor (called the Latent Phase) is best experienced
in the comfort of your home.
When the cervix dilates
from 4 to 8 centimeters (called the Active Phase), contractions get
stronger and are about 3 minutes apart, lasting about 45 seconds. You
may have a backache and increased bleeding from your vagina
(called the "bloody show"). Your mood may become more serious as you
focus on the hard work of dealing with the contractions. You will also
depend more on your support person.
Tips to help you through the Active Phase of labor:
- Try changing your position. You may want to try getting on your hands and knees to ease the discomfort of back labor.
- Soak in a warm tub or take a warm shower.
- Continue practicing breathing and relaxation techniques.
If
your amniotic membrane ruptures -- or your "water breaks" -- the
contractions may get much stronger. When the cervix dilates from 8 to 10
centimeters (called the Transition Phase), contractions are 2 to 3
minutes apart and last about 1 minute. You may feel pressure on your
rectum and your backache may feel worse. Bleeding from your vagina will be heavier.
It may help to practice breathing and relaxation techniques such as massage
or listening to soothing music. Focus on taking one contraction at a
time. Remember that each contraction brings you closer to holding your
baby.
It is during the active phase of labor that you
will go to the hospital or birthing center. Upon arrival, you will be
asked to wear a hospital gown. Your pulse, blood pressure, and temperature will be checked. A monitor will be placed on your abdomen for a short time to check for uterine contractions and assess the baby's heart rate. Your health care provider will also examine your cervix during a pelvic exam to determine how far labor has progressed.
An intravenous (IV) line may be placed into a vein in your arm to deliver fluids and medications if necessary.
The Second Stage of Labor (Delivery)
The
second stage of labor begins when your cervix is fully dilated at 10
centimeters. This stage continues until your baby passes through the
birth canal, vagina, and is born. This stage may last two hours or
longer.
Contractions may feel different from the
first stage of labor -- they will slow to 2 to 5 minutes apart and last
from about 60 to 90 seconds. You will feel a strong urge to push with
your contractions. Try to rest as much as possible between intervals of
pushing, and only push when the health care provider tells you.
Tips to help you push:
- Try several positions -- squatting, lying on your side with your leg up, or resting on your hands and knees.
- Take deep breaths in and out before and after each contraction.
- Curl into the push as much as possible; this allows all of your muscles to work.
You
may receive pain-relieving medications or have an episiotomy if
necessary while pushing. An episiotomy is a procedure in which a small
incision is made between the anus
and vagina to enlarge the vaginal opening. An episiotomy may be
necessary to assist the baby out quicker or to prevent large, irregular
tears of the vaginal wall.
The location of your
baby's head as it moves through the pelvis (called descent) is reported
in a number called a station. If the baby's head has not started its
descent, the station is described at minus 3 (-3). When your baby's head
is at the zero station, it is at the middle of the birth canal and is
engaged in the pelvis. The station of your baby helps indicate the
progress of the second stage of labor.
When your baby is born, your health care provider will hold the baby with his or her head lowered to prevent amniotic fluid, mucus, and blood from getting into the baby's lungs. The baby's mouth
and nose will be suctioned with a small bulb syringe to remove any
additional fluid. Your health care provider will place the baby on your stomach and shortly after, the umbilical cord will be cut.
The Third Stage of Labor
The
third stage of labor begins after the baby is born and ends when the
placenta separates from the wall of the uterus and is passed through the
vagina. This stage is often called delivery of the "afterbirth" and is
the shortest stage of labor. It may last from a few minutes to 20
minutes. You will feel contractions but they will be less painful. If
you had an episiotomy or small tear, it will be stitched during this
stage of labor.
Delivery of Your Premature Infant
A premature
delivery may happen suddenly or after days or weeks of waiting and worrying. If
you know you may deliver early, you, your partner, and your doctor can prepare
for a premature birth.
The premature delivery
You and your
premature infant (preemie) are considered high-risk
during preterm labor. This means that you will have less freedom, both to make
birth-related decisions and to move about freely. You can expect the
following:
- You may need to adjust your birth plan and birthing choices during this birth. You can refuse medicines such as painkillers during preterm labor. But other treatments such as antibiotics or corticosteroids can be important to ensure your infant's chances of good health after birth. Be sure to ask as many questions as you can think of about your medical care. The more you understand about your doctor's decisions, the less anxious you will feel.
- You will be on constant fetal heart monitoring. You also will be checked regularly for changes in heart rate, body temperature, and uterine contractions.
- You will probably deliver vaginally, rather than by cesarean section (C-section), as long as you and your fetus show no signs of distress.
After the premature birth: The infant
As soon as
the
umbilical cord is cut, the neonatal staff will
watch over and stabilize your infant. If your infant is less than 36 weeks'
gestation
at birth, they may move him or her to the neonatal
intensive care unit (NICU) for observation and specialized care. If
you deliver in a hospital that has no NICU, your infant may need to be
taken to another hospital.
During the first hours and
days, your infant will adjust to living outside of the maternal "life-support
system." This is a time when birth defects and complications of prematurity
often become apparent.
If your infant is
born between 22 and 25 completed weeks of pregnancy (extreme prematurity), you
likely will be faced with some
difficult decisions during the first month
after the birth. These
personal stories may help you make your decision.
After the premature birth: The mom
While the
neonatal staff attends to your infant, the obstetric staff will care for you.
Depending on your condition, this will take
at least a few hours. Meanwhile, your birth partner may want to go with your
infant to the NICU.
Before your breast milk comes in (3 or 4 days
after childbirth), you will be asked to decide whether you plan
to breast-feed or bottle-feed your premature infant. Formula does not give your infant added
protection from early infection, so strongly consider pumping
milk for your infant for at least the first weeks of life. If
you decide to breast-feed, expect at first to pump milk for feedings until your
infant is mature enough to feed orally.
- Breast milk contains antibodies that help protect your vulnerable infant against early, serious infections, including sepsis and necrotizing enterocolitis, as well as ear and upper respiratory infections during early childhood.
- The benefits of breast milk over formula include better nutrient absorption, digestive functioning, and nervous system development.
- Both specialized formula and breast milk can offer your infant excellent nutrition.
- Pumping and breast-feeding can be one of the most beneficial and rewarding things you do for your premature infant. But it may also be hard and exhausting. If you cannot breast-feed, decide not to breast-feed, or find that you have to discontinue doing so, formula feeding will meet your infant's nutritional needs.
Your
hospital's
lactation consultant can be very helpful with pumping
and breast-feeding questions and problems, both before and after the birth.













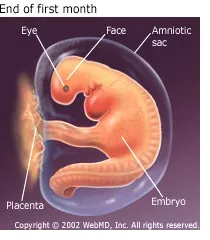





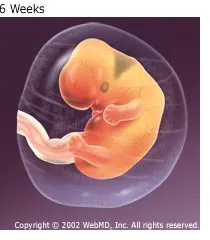
































































The extra time and effort you put in is certainly worthwhile. Wonderful work! Thanks!
ReplyDeleteHere is a great herbal doctor who cured me of Hepatitis B. his name is Dr. Imoloa. I suffered Hepatitis B for 11 years, I was very weak with pains all over my body my stomach was swollen and I could hardly eat. And one day my brother came with a herbal medicine from doctor Imoloa and asked me to drink and I drank hence there was no hope, and behold after 2 week of taking the medicine, I started feeling relief, my swollen stomach started shrinking down and the pains was gone. I became normal after the completion of the medication, I went to the hospital and I was tested negative which means I’m cured. He can also cure the following diseases with his herbal medicine...lupus, hay fever, measles, dry cough, diabetics hepatitis A.B.C, mouth ulcer, mouth cancer, bile salt disease, fol ate deficinecy, diarrhoea, liver/kidney inflammatory, eye cancer, skin cancer disease, malaria, chronic kidney disease, high blood pressure, food poisoning, parkinson disease, bowel cancer, bone cancer, brain tumours, asthma, arthritis, epilepsy, cystic fibrosis, lyme disease, muscle aches, fatigue, muscle aches, shortness of breath, alzhemer's disease, acute myeloid leukaemia, acute pancreatitis, chronic inflammatory joint disease, Addison's disease back acne, breast cancer, allergic bronchitis, Celia disease, bulimia, congenital heart disease, cirrhosis, constipation, fungal nail infection, fabromyalgia, (love spell) and many more. he is a great herbalist man. Contact him on email; drimolaherbalmademedicine@gmail.com. You can also reach him on whatssap- +2347081986098.
ReplyDeleteGood news this is to everyone out there with different health challenges, as I know there are still a lot of people suffering from different health issues and are therefore looking for solutions. I bring you Good news. There is a man called Dr ehiaguna a herbal practitioner who helped cure me from HSV (2), i had suffered from this diseases for the past 5 years and i have spent so much money trying to survive from it. I got my healing by taking the herbal medicine Dr ehiaguna sent to me to drink for about 14 days . 3 days after completion of the dosage, I went for a medical checkup and I was tested free from HSV. all thanks to God for leading me to Dr ehiaguna who was able to cure me completely from this deadly diseases, I’m sharing this so that other people can know of this great healer called Dr ehiaguna because I got to know him through elizabeth who he cured from HIV. I was made to understand that he can cure several other deadly diseases and infections. Don’t die in ignorance or silent and don’t let that illness take your life. Contact Dr ehiaguna through his emaildrehiaguna@gmail.com You can also whatsapp/call him on:+2348073908953 .He cure all forms of disease {1}HIV/AIDS {2}DIABETES {3}EPILEPSY {4} BLOOD CANCER {5} HPV {6} BRAIN TUMOR {7} HEPATITIS {8}COPD{9} SICKLE AND ANAEMIA.etc Be kind enough to share as you received.
ReplyDelete